On November 22, 2022, the Health and Resources and Services Administration (HRSA) issued a notice seeking nominations of qualified candidates for consideration to serve as members of the Advisory Committee on Infant and Maternal Mortality (ACIMM). ACIMM advises the Secretary of Health and Human Services (HHS) (Secretary) on department activities, partnerships, policies, and programs directed at reducing infant mortality, maternal mortality and severe maternal morbidity, and improving the health status of infants of women before, during, or after pregnancy. Written nominations for membership on the ACIMM must be received on or before January 23, 2022, and nomination packages must be submitted electronically as email attachments to Vanessa Lee, MPH, the ACIMM’s Designated Federal Official, at: SACIM@hrsa.gov. NCUIH strongly encourages UIO staff working in the areas of infant and maternal health to submit nomination materials.
Background
The ACIMM was established in 1991 and advises the Secretary on department activities, partnerships, policies, and programs directed at reducing infant mortality, maternal mortality and severe maternal morbidity, and improving the health status of infants and women before, during, and after pregnancy. The ACIMM provides advice on how to coordinate federal, state, local, tribal, and territorial governmental efforts designed to improve infant mortality, related adverse birth outcomes, and maternal health, as well as influence similar efforts in the private and voluntary sectors. The ACIMM provides guidance and recommendations on the policies, programs, and resources required to address the disparities and inequities in infant mortality, related adverse birth outcomes and maternal health outcomes, including maternal mortality and severe maternal morbidity. With its focus on underlying causes of the disparities and inequities seen in birth outcomes for women and infants, the ACIMM advises the Secretary on the health, social, economic, and environmental factors contributing to the inequities and proposes structural, policy, and/or systems level changes. The ACIMM meets approximately four times per year, or at the discretion of the Designated Federal Officer in consultation with the Chair.
Nomination Eligibility and Information
HRSA is requesting nominations for voting members to serve as Special Government Employees (SGEs) on the ACIMM to fill open positions. The Secretary appoints ACIMM members with the expertise needed to fulfill the duties of the Advisory Committee. Nominees sought are medical, technical, or scientific professionals with special expertise in the field of maternal and child health, in particular, infant and/or maternal mortality and related health disparities; members of the public having special expertise about or concern with infant and/or maternal mortality; and/or representatives from such public health constituencies, consumers, and medical professional societies. Interested applicants may self-nominate or be nominated by another individual or organization.
Individuals selected for appointment to the Committee will be invited to serve for up to 4 years. Members appointed as SGEs receive a stipend and reimbursement for per diem and travel expenses incurred for attending ACIMM meetings and/or conducting other business on behalf of the ACIMM, as authorized by 5 U.S.C. 5703 for persons employed intermittently in government service
Nomination Package Materials
The following information must be included in the package of materials submitted for each individual nominated for consideration:
- A statement that includes the name and affiliation of the nominee and a clear statement regarding the basis for the nomination, including the area(s) of expertise and/or experience that may qualify a nominee for service on the ACIMM, as described above;
- confirmation the nominee is willing to serve as a member of the ACIMM;
- the nominee’s contact information (please include home address, work address, daytime telephone number, and an email address); and
- A current copy of the nominee’s curriculum vitae or resume. Nomination packages may be submitted directly by the individual being nominated or by the person/organization recommending the candidate.
Individuals who are selected to be considered for appointment will be required to provide detailed information regarding their financial holdings, consultancies, and research grants or contracts. Disclosure of this information is required in order for HRSA ethics officials to determine whether there is a potential conflict of interest between the SGE’s public duties as a member of the ACIMM and their private interests, including an appearance of a loss of impartiality as defined by federal laws and regulations, and to identify any required remedial action needed to address the potential conflict.
AI/AN Infant and Maternal Health
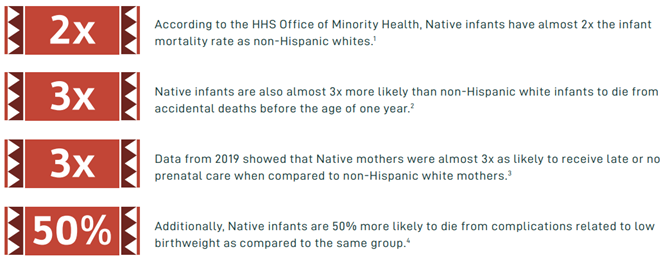
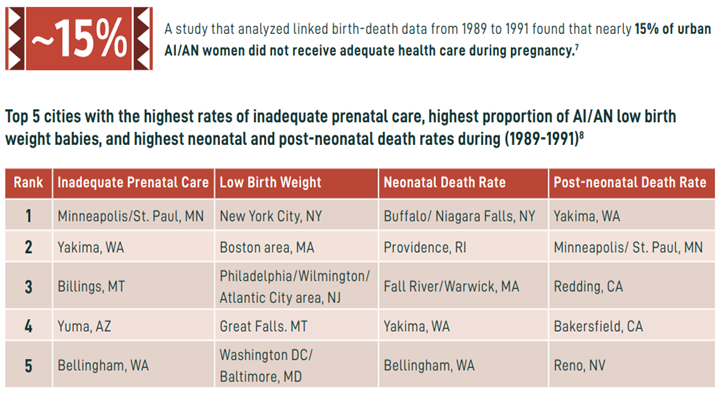
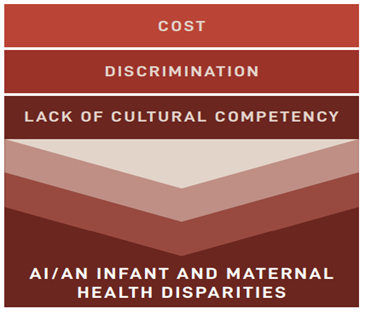
AI/AN communities throughout the country, including urban AI/AN communities, experience significant maternal and infant health disparities compared to the general population. According to HHS’ Office of Minority Health (OMH), AI/AN infants have almost twice the infant mortality rate as non-Hispanic whites. Native infants are also almost three times more likely than non-Hispanic whites to die from accidental deaths before the age of one year. Contributing factors to these disparities include cost, discrimination, and lack of cultural competency during prenatal care. Additional ongoing and historical trauma due to colonization, genocide, forced migration, and cultural erasure also contribute to health inequities, including pregnancy-related deaths and other maternal health conditions. Approximately 41% of AI/AN women cite cost as a barrier to receiving the recommended number of prenatal visits and 23% of AI/ANs report they have faced discrimination in clinical settings due to being an AI/AN. Consequently, AI/AN people are more likely to have underlying chronic health conditions, and they face systemic barriers to care including higher rates of poverty and needing to travel long distances to receive quality health care services.
Recognizing the infant and maternal health disparities that AI/AN people and communities experience, the HHS Secretary Xavier Becerra attended the White House Tribal Nations Summit on December 1, 2022, where he discussed the Department’s commitment to addressing mental and maternal health in AI/AN communities. As part of HHS’ commitment, the Centers for Disease Control and Prevention (CDC) and the Office of Minority Health (OMH) launched a new Hear Her campaign segment that works to improve AI/AN maternal health outcomes by raising awareness of life-threatening warning signs during and after pregnancy and improving communication between health care providers and their patients. Given HHS’ current focus on addressing Native infant and maternal health, it is highly recommended that UIO staff submit applications to the ACIMM to ensure that the voice of urban Native communities continues to be heard in this work.
UIO and NCUIH work in AI/AN Infant and Maternal Mortality
UIOs provide a range of services such as primary care, behavioral health, and traditional, and social services— including those for infants, children, and mothers. Several UIOs provide care for maternal health, infant health, prenatal, and/or family planning. They also provide pediatric services and participate in maternal-child care programs such as WIC and the Health Resources and Services Administration (HRSA) Maternal, Infant, and Early Childhood Home Visiting program (MIECHV).
NCUIH has engaged in extensive policy work on behalf of AI/AN mothers and infants and for increased funding and support to the UIOs which provide maternal health, infant health, prenatal, and family planning services to AI/AN mothers and infants. On March 9, 2022, NCUIH signed on to a letter to Congress led by the National Home Visiting Coalition in support of reauthorizing HRSA’s MIECHV and doubling the Tribal set-aside— which includes UIOs.
Also, in March, NCUIH submitted comments to the ACIMM, and on September 14, 2022, NCUIH’s Vice President of Public Policy, Meredith Raimondi, testified before the ACIMM on urban Indian disparities and policy changes to address these disparities. Raimondi highlighted that “over half of urban Indian health centers provide care for maternal health, infant health, prenatal, and/or family planning. However, due to chronic underfunding, many of these health centers only have the capacity to carry out these services for the early stages of pregnancy.” She continued to say, “despite desiring to do so, many urban Indian health clinics cannot expand their services to provide complete care for mothers and infants from conception to birth due to underfunding.” Raimondi provided the following recommendations to the Advisory Committee:
- Reauthorize MIECHV at a higher amount and double the Tribal set-aside from 3% to 6%.
- ACIMM and other stakeholders should collaborate with UIOs to gather critical and accurate information on urban AI/AN populations.
- Advise the HHS Secretary to lead the establishment of an urban confer policy across all HHS agencies.
- Include a Tribal and UIO health provider representative on the ACIMM and create an ACIMM subcommittee dedicated to addressing AI/AN infant and maternal health disparities.
In August, NCUIH submitted comments to HRSA’s Maternal and Child Health Bureau (MCHB) regarding the Pediatric Mental Health Care Access Program. In our comments, we have continued to stress the critical importance of including urban Natives populations in HRSA’s overall efforts of improving health outcomes for all AI/ANs living on and off reservations.
Furthermore, NCUIH recently released an infographic showcasing data on infant and maternal health disparities in American Indian/Alaska Native (AI/AN) communities.

 Raimondi highlighted that “over half of urban Indian health centers provide care for maternal health, infant health, prenatal, and/or family planning. However, due to chronic underfunding, many of these health centers only have the capacity to carry out these services for the early stages of pregnancy.” She continued to say, “despite desiring to do so, many urban Indian health clinics cannot expand their services to provide complete care for mothers and infants from conception to birth due to underfunding.” Raimondi provided the following recommendations to the Advisory Committee:
Raimondi highlighted that “over half of urban Indian health centers provide care for maternal health, infant health, prenatal, and/or family planning. However, due to chronic underfunding, many of these health centers only have the capacity to carry out these services for the early stages of pregnancy.” She continued to say, “despite desiring to do so, many urban Indian health clinics cannot expand their services to provide complete care for mothers and infants from conception to birth due to underfunding.” Raimondi provided the following recommendations to the Advisory Committee: