On December 5, 2022, Senator Elizabeth Warren (D-MA) and Representative Derek Kilmer (D-WA-6) introduced the Honoring Promises to Native Nations Act, which will address the underfunding and barriers to sovereignty in Indian Country acknowledged in the 2018 U.S. Commission on Civil Rights report, Broken Promises: Continuing Federal Funding Shortfall for Native Americans. The legislation reaffirms the federal government’s trust obligation to all American Indians and Alaska Natives (AI/ANs) to strengthen federal programs and support Native Communities. This legislation guarantees mandatory, full, and inflation-adjusted funding that can support healthcare, education, housing, and economic development and is cosponsored by national Indian organizations such as the National Council of Urban Indian Health (NCUIH), the National Congress of American Indians, and the National Indian Health Board.
NCUIH worked closely with Senator Warren’s office on this landmark policy platform, which includes permanent 100% Federal Medical Assistance Percentage (FMAP) for urban Indian organizations (UIOs) and modifying an existing policy to allow the Secretary of the Department of Health and Human Services (HHS) to better communicate on issues affecting urban Indian health. Additionally, the legislation includes mandatory-adjusted funding for the Indian Health Service (IHS), advance appropriations for IHS, increased long-term funding for Special Diabetes Programs for Indians (SDPI) to $300 million through fiscal year (FY) 2032 (currently expiring in FY 2023 and only funded at $150 million annually), and exempting Indian programs from sequestration.
“For generations, the U.S. government has clearly failed to fulfill its commitments to Tribal Nations. This bill is sweeping in ambition to make good on those commitments and empower Native communities, and it provides a much-needed legislative blueprint to deliver significant, long-term funding for the advancement of Native Americans. I won’t stop fighting to ensure the U.S. government honors its promises,” said Senator Warren.
“Congress and the federal government have a moral and a legal obligation to fulfill the promises made to Indian Country. That’s why I’m proud to introduce this legislation with Senator Warren to help reverse the decades-long pattern of systemic funding shortfalls to Native communities and to strengthen federal programs that support Indian Country. Congress should move swiftly to get this legislation enacted. It is long overdue.” said Representative Kilmer. “
“The health of our people has suffered due to the failure of the government to uphold the trust responsibility of providing health care to all American Indians and Alaska Natives. It is time that we address the needs of Indian Country and enact the recommendations included in the 2018 Broken Promises report, including improving health care for all Native people. The National Council of Urban Indian Health is grateful for the inclusion of Urban Indians in this legislation, especially regarding permanent 100% FMAP for urban Indian organizations and Urban Confer within HHS, both of which have been top priorities for NCUIH. We fully support this bill and believe that this Act is fundamental in honoring the federal government’s trust responsibility to American Indian and Alaska Natives,” – Francys Crevier (Algonquin), CEO, NCUIH.
“On behalf of the nearly 1/4 UIOs in California, CCUIH endorses the Honoring Promises to Native Nations Act because it will increase health access for American Indians no matter where they live. California is home to the largest population of American Indians, with more than 90% living in an urban area. Full, mandatory, inflation-adjusted funding for the Indian Health Service; funding for the Special Diabetes Programs for Native Americans; permanent FMAP for Urban Indian Health Programs; and Medicaid coverage of any services provided by Indian health care providers will offer critical funding necessary to address the continued disparities in health experienced by American Indians,” – Virginia Hedrick (Yurok), Executive Director, California Consortium for Urban Indian Health, Inc.
“The American Indian Health Service of Chicago, Inc. is pleased to endorse the Honoring Promises to Native Nations Act, as it will enable the 70% of American Indians and Alaska Natives who live in Urban Areas to continue to receive the same level of care that is received by other federally funded health programs, while slowly moving toward true health equity with the rest of the United States. With hope that Urban Programs will be able to receive an increase in the funding to be able to offer additional services (such as dental, podiatry, imaging, and women’s wellness) to the American Indian and Alaska Native Chicago based population. AIHSC also appreciates the efforts to increase the Special Diabetes Program for Indians, as our percentages of AI/AN who are diagnosed with diabetes increase,” – RoxAnne M LaVallie-Unabia (Turtle Mountain Band of Chippewa Indians), Executive Director, American Indian Health Service of Chicago.
“South Dakota Urban Indian Health enthusiastically supports the Honoring Promises to Native Nations Act. This bill secures funding for essential health services and through the inclusion of Medicaid reimbursements for substance use disorder facilities, recognizes the urgency of addiction for our relatives. For generations, Native Americans have persevered through forced assimilation, forced removal from our ancestral lands, and broken promises from the United States government. Despite these challenges, we remain a thriving group of sovereign nations and peoples across the geographic United States. This bill is a stride toward health equity for the more than 70% of Native Americans who live in urban areas of the United States.” – Michaela Seiber (Sisseton-Wahpeton Dakota), CEO, South Dakota Urban Indian Health.
“Native Health endorses the Honoring Promises to Native Nations Act because it will provide resources to fulfill the Federal Government’s obligation to provide health care to AI/ANs. The bill supports urban Indian organizations through 100% FMAP and SDPI reauthorization. These measures are especially needed by the underserved AI/AN urban community. In the current environment, UIOs are overwhelmed by the rising demand and the rising costs of providing health care,” – Walter Murillo (Choctaw Nation of Oklahoma), CEO, Native Health.
“The Honoring Promises to Native Nations Act is a major step forward in recognizing the trust and treaty obligations to Tribes and American Indian and Alaska Native peoples,” – Jacqueline Mercer, CEO, Native American Rehabilitation Association of the Northwest (NARA).
“Hunter Health endorses the Honoring Promises to Native Nations Act because it will increase access to quality healthcare services and allows Urban Indian Organizations to work with their state to expand services for Native American people living in their community,” – Rachel Mayberry, Chief Advancement Officer, Hunter Health.
“The Indian Health Center of Santa Clara Valley is pleased to endorse Senator Warren’s Honoring Broken Promises Act. This bill addresses priorities for urban Indian organizations such as mandatory funding, 100% FMAP, increased SDPI funding, and urban confer. This bill contributes to health equity for American Indians and Alaska Natives and moves forward with the federal government’s trust and treaty responsibility by improving AI/AN health services,” – Sonya Tetnowski (Makah), CEO, Indian Health Center of Santa Clara Valley.
“Denver Indian Health and Family Services endorses the Honoring Promises to Native Nations Act because it will allow all Urban Indian Organizations (UIOs) to leverage their services and sustain their funding despite many healthcare challenges. (i.e., the pandemic, the opioid crisis, suicide prevention, etc.). It is time the federal government met its trust and treaty obligations to Native peoples, particularly regarding federal spending. Failing to fund Indian Health Service (IHS) fully and UIOs fails to fulfill the federal government’s trust responsibilities. As recipients of less than 1% of the Indian Health Service budget, inadequate funding requires UIOs to depend on every dollar of federal funding and find creative ways to stretch limited resources. The Act will cover a wide range of issues that impact Indian Country; specifically, urban confer for HHS and the VA; 100% FMAP for UIOs; and Special Diabetes for Indians, reauthorized at $300 million for ten years,” – Adrianne Maddux (Hopi Tribe), Executive Director, Denver Indian Health and Family Services.
“The Oklahoma City Indian Clinic (OKCIC) endorses the Honoring Promises to Native Nations Act because it will provide promised and necessary funding for Indian Health Care services. The OKCIC is the largest Urban Indian Health Care Center in the United States, serving 22,000 patients from over 200 Tribes. Many of our patients are chronically ill and require high levels of expensive medical care. To provide that care it is very important that Title II of the Honoring Promises to Native Nations Act, specifically a full, mandatory and inflation-adjusted funding for the Indian Health Service and permanent adequate funding for the Special Diabetes Program for Indians is not only necessary but vital to maintaining the good health of our people,” – Robyn Sunday-Allen (Cherokee), CEO, Oklahoma City Indian Clinic.
Bill Highlights for Urban Indian Organizations
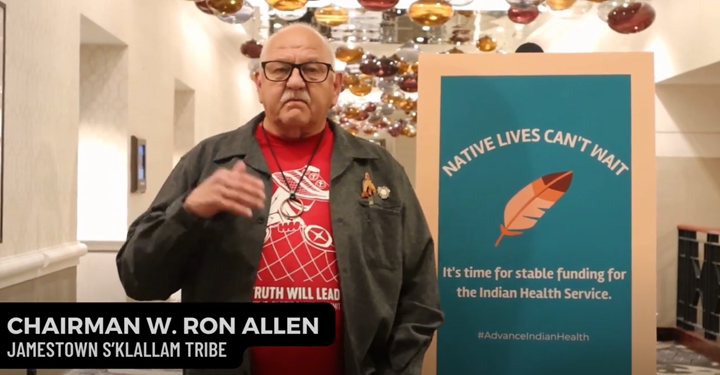
Mandatory Funding and Advance Appropriations for the Indian Health Service
The Indian health system, including IHS, Tribal facilities, and UIOs, is the only major federal provider of health care that is funded through annual appropriations. If IHS were to receive mandatory funding or, at the least, advance appropriations, it would not be subject to the harmful effects of government shutdowns and continuing resolutions (CRs) as its funding for the next year would already be in place. This is needed as lapses in federal funding put lives at risk. Without funding certainty during government shutdowns can cause UIOs to reduce services, close their doors, or force them to leave their patients without adequate care. During the last government shutdown, UIOs reported at least 5 patient deaths and significant disruptions in patient services. Securing stable funding for IHS has been a major priority for Indian Country and NCUIH has taken part in extensive advocacy to ensure the continuation and delivery of health services to all Native people regardless of where they live.
This bill authorizes $50,138,679,000 in mandatory appropriations for FY 2023, $51,416,373,000 for FY 2024, and for FY 2025 and each fiscal year thereafter, “an amount equal to the sum of the amount appropriated for the previous fiscal year, as adjusted annually to reflect the change in the medical care component of the consumer price index for all urban consumers (U.S. city average); and, as applicable, 1.8 percent of the amount appropriated for the previous fiscal year.” The bill also provides advance appropriations for IHS.
Special Diabetes Programs for Indians
The SDPI Demonstration Project includes research-based interventions for diabetes prevention and cardiovascular disease (CVD) risk reduction into AI/AN community-based programs and health care settings. The program has demonstrated success with a 50% reduction in diabetic eye disease rates, drops in diabetic kidney failure, and a 50% decline in End Stage Renal Disease. Many UIOs receive SDPI funding and the program has directly enabled UIOs to provide critical services to their AI/AN patients, in turn significantly reducing the incidence of diabetes and diabetes-related illnesses among urban Indian communities. These successes are impactful, as AI/ANs have the highest diabetes prevalence rates of all racial and ethnic groups in the United States, with AI/AN adults almost three times more likely than non-Hispanic white adults to be diagnosed with diabetes. According to the Centers for Disease Control and Prevention, 13.7% of adults in urban Native communities are diagnosed with diabetes. SDPI is a critical program to address the high rates of diabetes among AI/ANs and requires secure funding to continue its success. NCUIH has long advocated for SPDI to be fully funded. On May 16, 2022, NCUIH submitted comments and recommendations to IHS emphasizing the importance of SDPI in reducing health disparities related to diabetes for AI/AN populations. These comments included increasing SDPI funding with built-in automatic annual medical inflationary increases and that IHS ensures the SDPI remains inclusive of UIOs.
This legislation will reauthorize SDPI at $300,000,000 for each fiscal year beginning in 2023 through 2032.
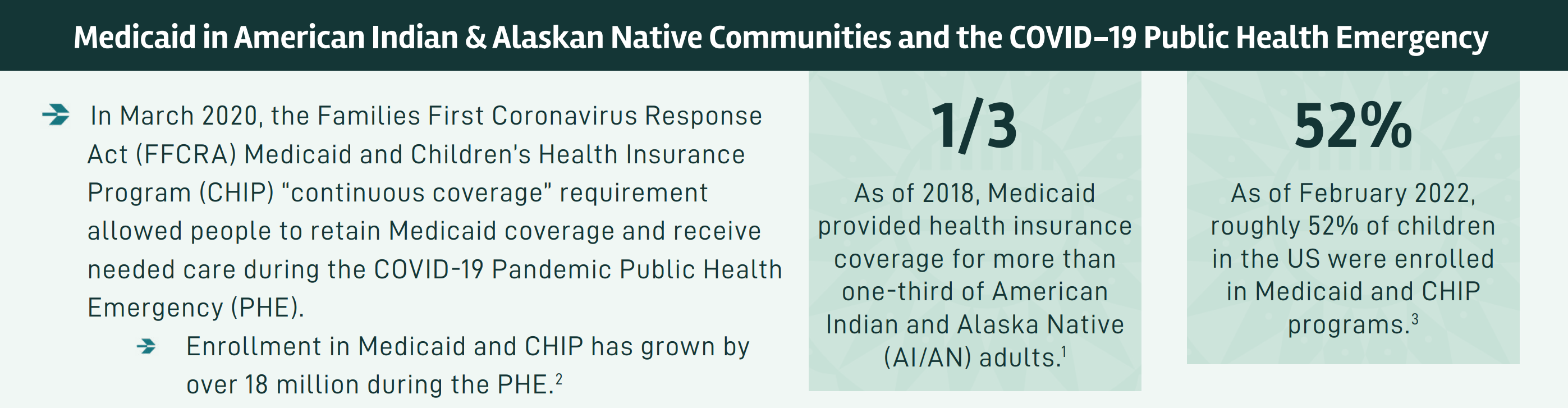
Permanent 100% Federal Medical Assistance Percentage (FMAP)
FMAP refers to the percentage of Medicaid costs covered by the federal government, which will be reimbursed to the states. Permanent 100% FMAP for UIOs will further the government’s trust responsibility to AI/ANs by increasing available financial resources to UIOs and support them in addressing critical health needs of AI/AN patients. In March of 2021, Congress enacted the American Rescue Plan Act of 2021 (ARPA) which authorized eight fiscal quarters of 100% FMAP coverage for UIOs. Unfortunately, with only 3 months until the provision expires, most UIOs have not received any increase in financial support because many states have not increased their Medicaid reimbursement rates to UIOs, citing short-term authorization concerns.
There has been strong support for the expansion of 100% FMAP to UIOs across Indian Country and NCUIH has tirelessly advocated to permanently fix this parity issue. The National Congress of American Indians and the National Indian Health Board passed resolutions along with NCUIH in support of extending 100% FMAP to UIOs. Additionally, there has been longstanding bipartisan congressional support, with over 17 pieces of legislation having been introduced since 1999 on this issue. NCUIH recently sent a letter to the House Committee on Energy and Commerce leadership requesting a markup on the Improving Access to Indian Health Services Act (H.R. 1888), which would establish permanent 100% FMAP for services provided to AI/ANs Medicaid beneficiaries at UIOs.
This bill amends the Social Security Act by including UIOs as eligible entities to receive permanent 100% FMAP.
Urban Confer with HHS and UIOs
An Urban Confer is an established mechanism for dialogue between federal agencies and UIOs. Urban confer policies are a response to decades of deliberate federal efforts (i.e., forced assimilation, termination, relocation) that have resulted in 70% of AI/AN people living outside of Tribal jurisdictions, thus making Urban Confer integral to addressing the care needs of a majority of AI/ANs. An urban confer policy that includes all HHS agencies, including the Centers for Medicare & Medicaid Services (CMS), ensures that obstacles relating to programs and benefits that directly affect UIOs are addressed quickly so UIOs are better equipped to provide healthcare to their patients. NCUIH has long advocated for facilitating confer between numerous federal branches within HHS and UIO stakeholders. Currently, only IHS has a legal obligation to confer with UIOs. It is important to note that urban confer policies do not supplant or otherwise impact Tribal consultation and the government-to-government relationship between Tribes and federal agencies.
This bill would require the Secretary of HHS, to the maximum extent practicable, to confer with UIOs in carrying out the health services of the Department.
Office of Management and Budget Office of Native Nations
The bill establishes an Office of Native Nations within the Office of Management (OMB), which coordinates with the rest of OMB and the Executive branch on matters of funding for federal programs and policy affecting AI/ANs and Native Hawaiians. The Administrator, a career position, of the office is responsible for matters such as compiling data on all federal funding for federal programs affecting AI/ANs and Native Hawaiians; ensuring that the budget requests of IHS and the Bureau of Indian Affairs indicate how much funding is needed for programs affecting AI/ANs and Native Hawaiians to be fully funded and how far the federal government is from achieving that full funding; and preparing a crosscutting document each fiscal year containing detailed information, based on data from all federal agencies, on the amount of federal funding that is reaching Indian Tribes, tribal organizations, Native Hawaiian organizations, and UIOs. The bill directs the Administrator to consult with Indian Tribes, collaborate with Native Hawaiian organizations, and confer with UIOs annually to ascertain how the crosscutting document can be modified to make it more useful to Indian Tribes, Native Hawaiian organizations, and UIOs.
On September 12, 2022, after recommendations from NCUIH and Tribal leaders, the Biden administration created a position of a Tribal Policy Advisor within OMB to communicate the needs of Indian Country and AI/ANs. This position was an important first step in ensuring that Native voices are heard during the budget process, and we are grateful that this bill works to further consider the needs of Native programs in federal funding.
Next Steps
Senator Warren and Congressman Kilmer invite comments and feedback on how to refine and improve the legislation in the next Congress. Written input can be submitted at HonoringPromises@warren.senate.gov.
Background
Broken Promises
On December 20, 2018, the Broken Promises report was released and addressed areas where the federal government has failed to fulfill its trust responsibility, including criminal justice and public safety, health care, education, housing, and economic development. Specifically, the report requests advance appropriations for the IHS and funding to implement the Indian Health Care Improvement Act, including job training programs to address chronic shortages of health professionals in Indian Country and a mental health technician training program to address the suicide crisis in Indian Country. The report also recommends direct, long-term funding to Tribes, analogous to the mandatory funding Congress provides to support Medicare, Social Security, and Medicaid, avoiding pass-through of funds via states.
The proposal for this bill was first introduced in August 2019 by Congresswoman Deb Haaland (D- N.M.) and Senator Warren. Lawmakers then took feedback from tribal governments and citizens, tribal organizations, UIOs, experts, and other stakeholders which informed the development of this current legislation.