April Policy Updates: Take Action to Increase IHS Funding and More
In this Edition:
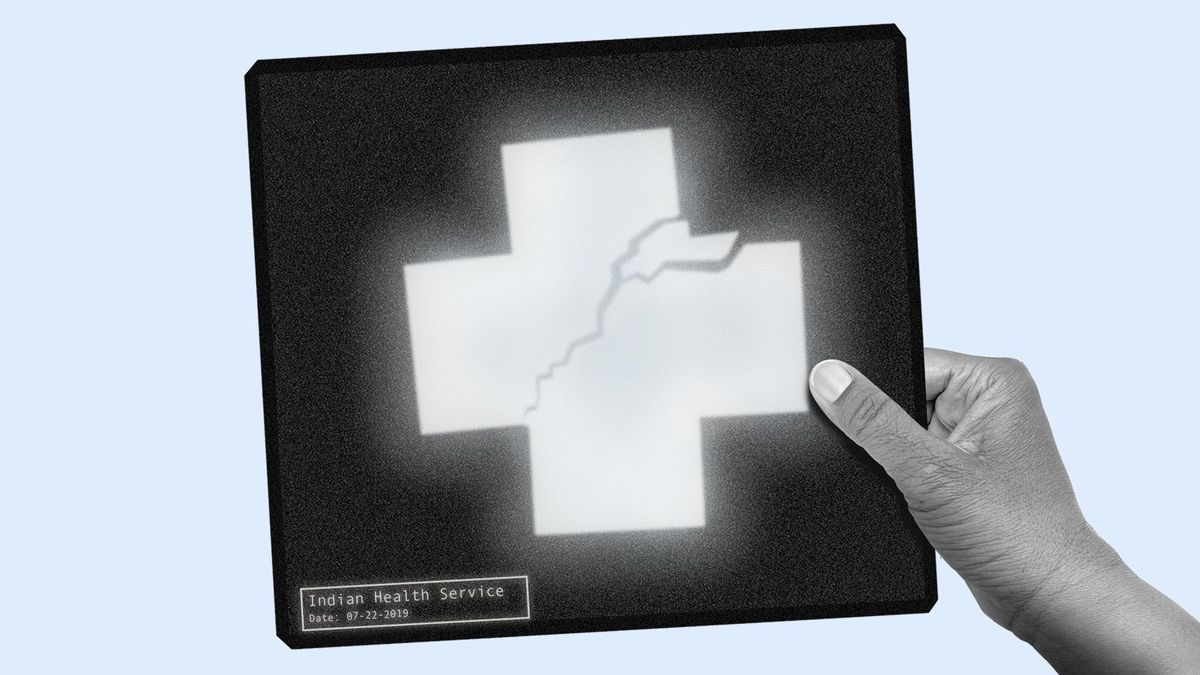
🗓 Take action to ask Congress for increased funding for the Indian Health Service.
🌍 Mark your calendars for upcoming meetings and comment opportunities.
🚀 Learn about our recent advocacy efforts.
Action Alert: Contact Congress to Increase Funding for Indian Health TODAY

We need your help contacting Congress to support access to health care for urban Native communities!
Representatives Ruben Gallego (D-AZ-03) and Raúl Grijalva (D-AZ-07) are leading a letter to the leadership of the Appropriations Subcommittee on Interior, Environment, and Related Agencies.
The letter calls for the highest possible funding for Urban Indian Health and Indian Health Service and recommends funding at $965.3 million and $53.85 billion, respectively.
- These amounts reflect the recommendations made by the Tribal Budget Formulation Workgroup.
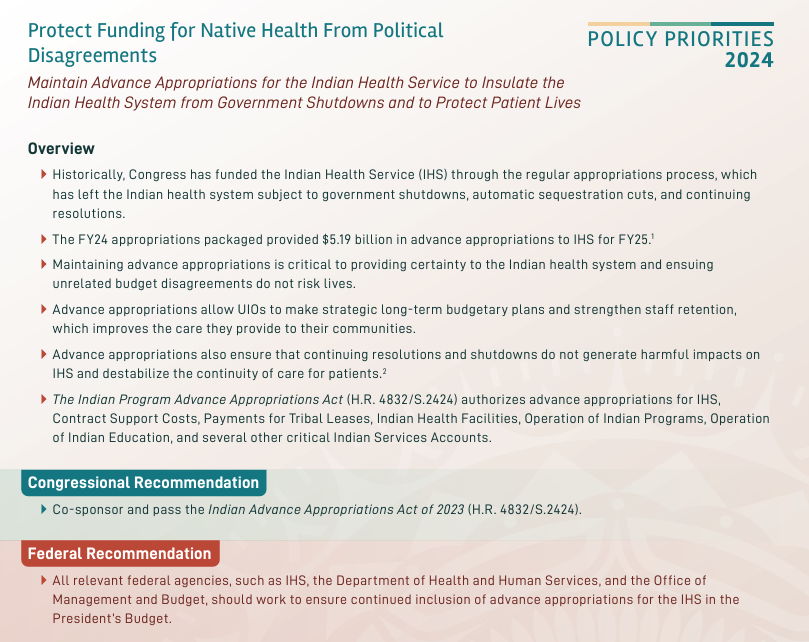
- The letter also calls for advance appropriations for IHS for FY 2026 and protection against sequestration in the final FY 2025 spending bill.
- To ensure that the Indian Health Service receives as much support as possible, we encourage you to contact your Member of Congress and request that they sign on to the Gallego-Grijalva Urban Indian Health letter.
Go deeper and find the text of the letter to send: Action Alert: Contact Congress to Increase Funding for Indian Health TODAY
NCUIH Participates in Congressional Roundtable to Advocate for Native Veterans

NCUIH was invited to participate in a roundtable to discuss critical health care issues facing urban Native veterans.
Go deeper: On April 16, Sonya Tetnowski, CEO of Indian Health Center of Santa Clara Valley and NCUIH Board President, attended a roundtable hosted by the House Committee on Veterans Affairs.
- The roundtable discussed issues facing Native veterans, equity in access to healthcare and benefits for veterans, and the state of cultural competency at the VA and community care providers.
Why it matters: NCUIH was able to discuss the importance of traditional healing for Native veterans and ensure that Congress understands the importance of the trust obligation for health care owed to all Native people, including our veterans.
New Resource: 2024 Policy Priorities Released
2024 Policy Priorities
The National Council of Urban Indian Health is pleased to announce the release of its 2024 Policy Priorities document.
- It outlines a summary of urban Indian organization (UIO) priorities for the Executive and Legislative branches of the government for 2024.
- These priorities were informed by NCUIH’s 2023 Policy Assessment.
NCUIH hosted five focus groups to identify UIO policy priorities for 2024, as they relate to Indian Health Service (IHS)- designated facility types (full ambulatory, limited ambulatory, outreach and referral, and outpatient and residential).
- NCUIH worked with UIOs to identify policy priorities in 2024 under eight themes.
The document contains talking points and recommendations for each priority.
Go deeper: Read the full priorities and the overview document.
NCUIH in Action: CEO Speaks at Native Youth Policy Panel

On April 26, Francys Crevier (Algonquin), JD, CEO was honored to join an impactful event with Native high school students organized by the Close Up Foundation in partnership with United South and Eastern Tribes.
- Francys joined an action expert panel, emphasizing the importance of involving youth in policy advocacy to address pressing community issues.

NCUIH Policy Analyst Emily Larsen at Budget Consultation.
On April 9 and 10, NCUIH represented Urban Indian Organizations at the Health and Human Services 26th Annual Tribal Budget Consultation.
Congressional Updates: FY25 American Indian and Alaska Native Witness Day and FY24 Health Budget News
On May 8, 2024, Todd Wilson, Executive Director of Helena Indian Alliance-Leo Pocha Clinic and NCUIH board member, will be NCUIH’s witness for the House Appropriations Committee’s American Indian and Alaska Native Witness Days.
What else?: On March 22, Congress passed the remaining 6 appropriations bills to fund the government for FY24.
- The Labor-Health and Human Services appropriations bill is included in this package.
Some highlights include:
- $6 million creation of an Initiative for Improving Native American Cancer Outcomes that includes Urban Indian Organizations.
- Level funding for HIV funding, including maintaining $5 million for the Tribal Set-aside for the Minority HIV/AIDS Prevention and Treatment program.
Monitoring the Bench: Becerra v. San Carlos Apache/Becerra v. Northern Arapaho Tribe (Consolidated)

Why it matters: This issue relates to federal responsibility to pay “contract support costs” to Tribes not only to support IHS-funded activities, but also to support the Tribe’s expenditure of third-party income.
What else?: NCUIH joined the Amicus Brief filed by the National Indian Health Board on February 19.
Did you know?: The oral Argument occurred March 25.
Go deeper: The Court appeared split on whether the federal government should be responsible. There is no good prediction for the outcome at this point
What’s next: Decision to be released by June 30, 2024.
Federal Update: Medicaid Coverage of Traditional Healing at IHS and Tribal Facilities
The Centers for Medicare and Medicaid Services (CMS) are seeking feedback on a proposed Traditional Healing Framework for section 1115 demonstrations.
- CMS is seeking advice and input on the scope of coverage of traditional health care practices that could be provided at IHS and tribal facilities, recommendations on provider qualifications, and monitoring and evaluation criteria.
- Through section 1115(a) demonstration authority, CMS can provide expenditure authority allowing a state to claim federal funding for new services not otherwise coverable under Medicaid.
- CMS recently provided an overview of the section 1115(a) demonstration process and a high-level overview of the four pending demonstration proposals to cover traditional health care practices.
- CMS discussed its framework for potential coverage of traditional health care practices, consistent with the authorities in the Indian Health Care Improvement Act.
Go deeper: The presented Framework does not include UIOs as eligible facilities under the proposed framework.
What’s New?: To allow more time for comments, the comment period has been extended to COB Friday, May 3, 2024.
- Please submit written comments to tribalaffairs@cms.hhs.gov.
Upcoming Events

Thank you for your advocacy and leadership! We look forward to seeing you in Washington, DC soon at our conference!