Resource: Data on Infant and Maternal Health Disparities in Native Communities
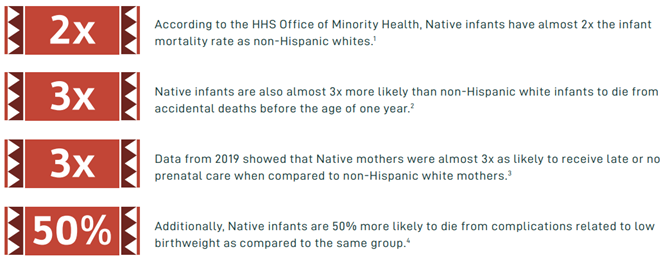
The National Council of Urban Indian Health (NCUIH) recently released an infographic showcasing data on infant and maternal health disparities in American Indian/Alaska Native (AI/AN) communities. Unfortunately, AI/AN communities throughout the country, including urban AI/AN communities, experience significant maternal and infant health disparities compared to the general population.
AI/AN Infant and Maternal Health Disparities
A report by the National Center for Health Statistics noted that between 2005 and 2014, American Indian/Alaska Native was the only racial or ethnic group that did not experience a decline in infant mortality.[1]
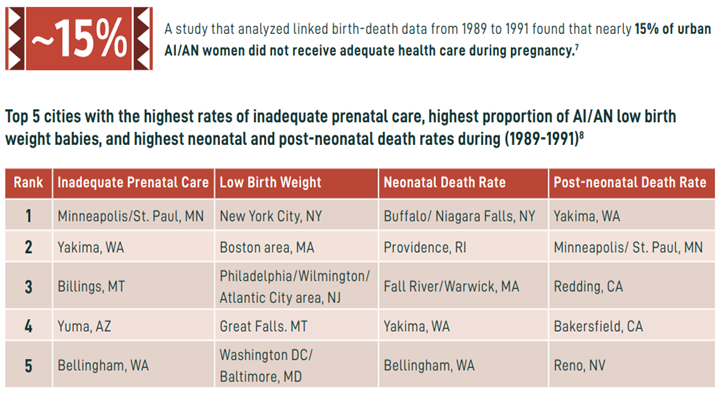
Urban AI/AN Infant and Maternal Health Disparities
Over half of urban Indian organizations (UIOs) provide care for maternal health, infant health, prenatal, and/or family planning. A study of Natives in UIO service areas found that while birth rates, in general, were lower in the urban Native population (12.8 and 16.5 per 1,000 population, respectively), premature birth rates for both urban and non-urban AI/AN were higher than those of all other races and ethnicities combined (12.3% of live births among AI/AI in urban areas and 10.9% among the general population in the same area).[2]
Contributing Factors to AI/AN Infant and Maternal Health Disparities
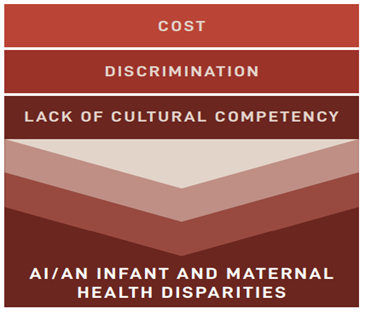
- Cost, discrimination, and lack of cultural competency are all contributing factors to the stark infant and maternal health disparities among AI/ANs.
- 41% of AI/AN women cite cost as a barrier to receiving the recommended number of prenatal visits.[3]
- AI/AN women are 3-4x more likely to begin prenatal care in the third trimester.[4]
- 21% of AI/AN women ages 15-44 are uninsured, compared to 8% of white women.[5]
- 23% of AI/ANs report they have faced discrimination in clinical settings due to being an AI/AN.[6]
- 15% report avoiding medical care for themselves or family members due to fear of discrimination.[7]
- Access to culturally appropriate care can be difficult for AI/ANs living in urban areas, as most IHS clinics and hospitals, as well as Tribal healthcare facilities, are located on reservations.[8]
UIO and NCUIH work in AI/AN Infant and Maternal Mortality
UIOs provide a range of services such as primary care, behavioral health, traditional, and social services— including those for infants, children, and mothers. At least 23 of these clinics provide care for maternal health, infant health, prenatal, and/or family planning. They also provide pediatric services and participate in maternal-child care programs such as WIC and the Health Resources and Services Administration (HRSA) Maternal, Infant, and Early Childhood Home Visiting program (MIECHV).
NCUIH has engaged in extensive advocacy on behalf of AI/AN mothers and infants and for increased funding and support to the UIOs which provide maternal health, infant health, prenatal, and family planning services to AI/AN mothers and infants. On March 9, 2022, NCUIH signed on to a letter to Congress led by the National Home Visiting Coalition in support of reauthorizing HRSA’s Maternal, Infant, and Early Childhood Home Visiting Program (MIECHV) and doubling the Tribal set-aside— which includes UIOs.
Also, in March, NCUIH submitted comments to the HRSA Advisory Committee on Infant and Maternal Mortality (ACIMM), which advises the Secretary of Health and Human Services (HHS) on department activities, partnerships, policies, and programs directed at reducing infant mortality, maternal mortality and severe maternal morbidity, and improving the health status of infants and women before, during, and after pregnancy. In August, NCUIH submitted comments to HRSA’s Maternal and Child Health Bureau (MCHB) regarding the Pediatric Mental Health Care Access Program in August. In our comments, we have continued to stress the critical importance of including urban Natives populations in HRSA’s overall efforts of improving health outcomes for all AI/ANs living on and off reservations.
On September 14, 2022, NCUIH’s Vice President of Public Policy, Meredith Raimondi, testified before the HRSA ACIMM on urban Indian disparities and policy changes to address these disparities.  Raimondi highlighted that “over half of urban Indian health centers provide care for maternal health, infant health, prenatal, and/or family planning. However, due to chronic underfunding, many of these health centers only have the capacity to carry out these services for the early stages of pregnancy.” She continued to say, “despite desiring to do so, many urban Indian health clinics cannot expand their services to provide complete care for mothers and infants from conception to birth due to underfunding.” Raimondi provided the following recommendations to the Advisory Committee:
Raimondi highlighted that “over half of urban Indian health centers provide care for maternal health, infant health, prenatal, and/or family planning. However, due to chronic underfunding, many of these health centers only have the capacity to carry out these services for the early stages of pregnancy.” She continued to say, “despite desiring to do so, many urban Indian health clinics cannot expand their services to provide complete care for mothers and infants from conception to birth due to underfunding.” Raimondi provided the following recommendations to the Advisory Committee:
- Reauthorize MIECHV at a higher amount and double the Tribal set-aside from 3% to 6%.
- ACIMM and other stakeholders should collaborate with UIOs to gather critical and accurate information on urban AI/AN populations.
- Advise the HHS Secretary to lead the establishment of an urban confer policy across all HHS agencies.
- Include a Tribal and UIO health provider representative on the ACIMM and create an ACIMM subcommittee dedicated to addressing AI/AN infant and maternal health disparities.
[1] Mathews TJ, Driscoll AK, Trends in infant mortality in the United States, 2005–2014, (2017) available at: https://www.cdc.gov/nchs/data/databriefs/db279.pdf
[2]Castor ML, Smyser MS, Taualii MM, Park AN, Lawson SA, Forquera RA. “A nationwide population-based study identifying health disparities between American Indians/ Alaska Natives and the general populations living in select urban counties.” Am J Public Health, 2006;96(5)
[3] National Partnership for Women and Families, American Indian and Alaska Native Women’s Maternal Health: Addressing the Crisis, (2019), https://www. nationalpartnership.org/our-work/resources/health-care/maternity/american-indian-and-alaska.pdf
[4] Urban Indian Health Institute, Community Health Profile: National Aggregate of Urban Indian Health Program Service Areas, (2016), http://www.uihi.org/wp-content/ uploads/2017/08/UIHI_CHP_2016_Electronic_20170825.pdf
[5] National Partnership for Women and Families, American Indian and Alaska Native Women Face Pervasive disparities in Access to Health Insurance, (2019), https:// www.nationalpartnership.org/our-work/resources/health-care/AIAN-health-insurance-coverage.pdf
[6] Harvard T.H. Chan School of Public Health, Poll finds more than one-third of Native Americans report slurs, violence, harassment, and being discriminated against in the workplace (2017), https://www.hsph.harvard.edu/news/press-releases/poll-native-americans-discrimination/
[7] Id.
[8] See Mental Health America, Native and Indigenous Communities and Mental Health – Prevalence, https://www.mhanational.org/issues/native-and-indigenouscommunities-and-mental-health (last accessed Aug. 20, 2022).








Leave a Reply
Want to join the discussion?Feel free to contribute!