On February 26, 2025, the National Council of Urban Indian Health (NCUIH) submitted written testimony to the Senate Committee on Indian Affairs (SCIA) regarding the 119th Congress Priorities for Indian Country. NCUIH requested in its testimony for protected funding for the Indian Health Service (IHS) and Urban Indian Health as well as increased resources for key health programs.
In the testimony, NCUIH requested the following:
- Protect Funding for the Indian Health Service and fund Urban Indian Health at $100 million for Fiscal Year (FY) 2026.
- Maintain Advance Appropriations for the Indian Health Service, until mandatory funding is achieved, and protect IHS from sequestration.
- Ensure Federal Policies Uphold Trust Obligations to American Indian and Alaska Native Communities.
- Reauthorize the Special Diabetes Program for Indians at $250 million.
- Appropriate $80 million for Behavioral Health and Substance Use Disorder Resources for Native Americans.
- Protect Medicaid and Authorize Permanent 100% Federal Medical Assistance Percentage for services provided at urban Indian organizations (UIOs).
- Allow U.S. Public Health Service Commissioned Officers detailed directly to UIOs.
- Fund the Initiative for Improving Native American Cancer Outcomes at $10 million for FY 2026.
Next Steps:
This testimony will be considered by the Senate Committee on Indian Affairs and used in the development of the Committee’s priorities. NCUIH will continue to advocate for these requests in the 119th Congress and work closely with SCIA members and their staff.
Full Text of Testimony:
My name is Francys Crevier, I am Algonquin and the Chief Executive Officer of the National Council of Urban Indian Health (NCUIH), a national representative advocating for the 41 Urban Indian Organizations (UIOs) contracting with the Indian Health Service (IHS) under the Indian Health Care Improvement Act (IHCIA) and the American Indians and Alaska Native patients they serve. On behalf of NCUIH and these 41 UIOs, I would like to thank Chairman Murkowski, Vice Chairman Schatz, and Members of the Committee for your leadership to improve health outcomes for urban Indians and for the opportunity to provide testimony. We respectfully request the following:
- Protect Funding for the Indian Health Service and fund Urban Indian Health at $100 million for FY26
- Maintain Advance Appropriations for the Indian Health Service, until mandatory funding is achieved, and protect IHS from sequestration.
- Ensure Federal Policies Uphold Trust Obligations to American Indian and Alaska Native Communities.
- Reauthorize the Special Diabetes Program for Indians at $250 million.
- Appropriate $80 million for Behavioral Health and Substance Use Disorder Resources for Native Americans.
- Protect Medicaid and Authorize Permanent 100% Federal Medical Assistance Percentage for services provided at UIOs.
- Allow U.S. Public Health Service Commissioned Officers detailed directly to UIOs
- Fund the Initiative for Improving Native American Cancer Outcomes at $10 million for FY26.
A Brief History on Urban Indian Organizations:
As a preliminary issue, “urban Indian” refers to any American Indian or Alaska Native (AI/AN) person who is living in an urban area, either permanently or temporarily. UIOs were created by urban AI/AN people with the support of Tribes, starting in the 1950s in response to severe problems with health, education, employment, and housing.1 Congress formally incorporated UIOs into the Indian Health System in 1976 with the passage of the Indian Health Care Improvement Act (IHCIA). Today, over 70% of AI/AN people live in urban areas. UIOs are an integral part of the Indian health system, comprised of the Indian Health Service, Tribes, and UIOs (collectively I/T/U), and provide essential healthcare services, including primary care, behavioral health, and social and community services, to patients from over 500 Tribes in 38 urban areas across the United States. UIOs also work closely with Tribal and law enforcement partners to address the Missing and Murdered Indigenous People’s (MMIP) crisis.
Request: Protect Funding for the Indian Health Service and fund Urban Indian Health at $100 million for FY26
The federal government owes a trust obligation to provide healthcare services to AI/AN people no matter where they live. In fact it is the national policy of the United States “to ensure the highest possible health status for Indians and urban Indians and to provide all resources necessary to effect that policy.”2 This requires that funding for Indian health be significantly increased if the federal government is to finally fulfill its trust responsibility. At a minimum, funding must be maintained and protected as budget-cutting measures are being considered.
Without an increase to the urban Indian health line item, UIOs will continue to be forced to operate on limited and inflexible budgets, that limit their ability to fully address the needs of their patients. A lack of federal funding is deeply impactful for UIOs who are on the front lines in working to provide for the health and well-being of American Indians and Alaska Natives living outside of Tribal jurisdictions. While UIOs historically only receive 1% of the IHS budget, they have been excellent stewards of the funds allocated by Congress and are effective at ensuring that increases in appropriations correlate with improved care for their communities.
We thus request Congress honor its trust obligation by appropriating the maximum amount possible for IHS and appropriating at least $100 million for Urban Indian Health, which is in line with the House proposed amount for FY25. As the Tribal Budget Formulation Workgroup (TBFWG) report states, “Only a significant increase to the Urban Indian Health line item will allow UIOs to increase and expand services to address the needs of their American Indian and Alaska Native patients, support the hiring and retention of culturally competent staff, and open new facilities to address the growing demand for UIO services.” Increased investments in Urban Indian Health will continue to result in the expansion of health care services, increased jobs, and improvement of the overall health in urban American Indian and Alaska Native communities.
Request: Maintain Advance Appropriations for the Indian Health Service until Mandatory Funding is Enacted and Protect Against Sequestration
The inclusion of advance appropriations in the FY24 Omnibus and maintaining advance appropriations for FY25, is a crucial step towards ensuring long-term, stable funding for IHS. Previously, the I/T/U system was the only major federal health care provider funded through annual appropriations. It is imperative that Congress maintain advance appropriations for the IHS in the final spending bill for FY26 and beyond. It is also imperative to protect IHS from sequestration.
Advance appropriations improve accountability and increase staff recruitment and retention at IHS. When IHS distributes their funding on time, our UIOs can consistently pay their doctors and providers.
It is also imperative to shield and protect the IHS from cuts or funding freezes that force Indian health-providers to make difficult decisions about the scope of healthcare services they can offer to American Indian and Alaska Native patients. For example, the sequestration of $220 million in IHS’ budget authority for FY 2013 resulted in an estimated reduction of 3,000 inpatient admissions and 804,000 outpatient visits for American Indian and Alaska Native patients.3 A recent survey from the National Council of Urban Indian Health, over half of surveyed UIOs report they would be unable to sustain operations beyond six months without federal funding.4 UIOs provide essential healthcare services to their patients, including primary care, urgent care, and behavioral health services, and are on the front lines in working to provide for the health and well-being of American Indian and Alaska Native people living in urban areas, many of whom lack access to the health care services that it is the federal government’s trust responsibility to provide. Any reduction or pause in funding would reduce UIOs’ ability to provide these essential services to their patients and communities, delaying care and reducing UIO capacity to take on additional patients.
Therefore, we request that you exempt IHS from sequestration in an amendment to Sec. 255 of the Balanced Budget and Emergency Deficit Control Act. We also request that IHS funding be protected from impoundment and other budget-cutting measures as is required by the trust responsibility.
Finally, while advance appropriations are a step in the right direction to avoid disruptions during government shutdowns and CRs, mandatory funding is the only way to assure fairness in funding and fulfillment of the trust responsibility. Until authorizers act to move IHS to mandatory funding, we request that Congress continue to provide advance appropriations to the Indian health system to improve certainty and stability.
Request: Ensure Federal Policies Uphold Trust Obligations to American Indian and Alaska Native Communities
We acknowledge and appreciate the recent steps taken by the Departments of Health and Human Services (HHS), Interior, and the Office of Personnel Management (OPM) to clarify that actions should not interfere with the United States’ commitment to fulfilling its trust obligations to American Indian and Alaska Native communities. However, we remain concerned that potential future actions may fail to adequately consider this unique relationship.
Therefore, we respectfully request that the Congress take necessary steps to ensure these directives are implemented in a manner consistent with the unique political status of American Indian and Alaska Native people under U.S. law, as well as the federal government’s legal obligation to uphold its trust responsibilities. Specifically, we request that Congress pass legislative text that explicitly exempts IHS from similar policies being applied across the federal government to safeguard the delivery of critical services to American Indian and Alaska Native people.
Request: Appropriate $80 Million for Behavioral Health and Substance Use Disorder Resources for Native Americans
In response to these chronic health disparities, Congress authorized $80 million to be appropriated for the Behavioral Health and Substance Use Disorder Resources for Native Americans Program for fiscal years 2023 to 2027. Despite authorizing $80 million for the Program, Congress has failed to appropriate funds for this program.
We request that the authorized $80 million be appropriated to the Behavioral Health and Substance Use Disorder Resources for Native Americans Program for FY25 and each of the remaining authorized years. Until Congress appropriates funding for this program, critical healthcare programs and services cannot operate to their full capability, putting American Indian and Alaska Native lives at-risk. This is an essential step to ensure our communities have access to the care they need.
Request: Reauthorize the Special Diabetes Program for Indians at $250 Million
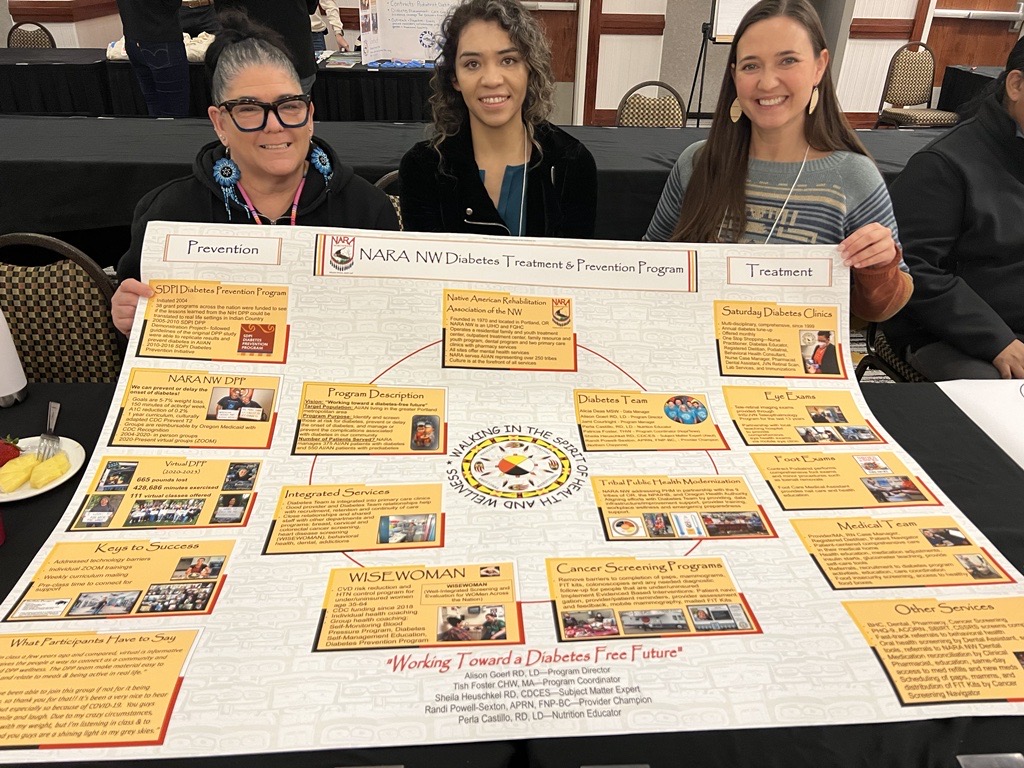
SDPI’s integrated approach to diabetes healthcare and prevention programs in Indian country has become a resounding success and is one of the most successful public health programs ever implemented. SDPI has demonstrated success with a 50% reduction in diabetic eye disease rates, drops in diabetic kidney failure, and 50% decline in End State Renal Disease.5 Additionally, the reduction in end stage renal disease between 2006 and 2015 led to an estimated $439.5 million dollars in accumulated savings to the Medicare program, 40% of which, of $174 million, can be attributed to SDPI.6
Currently 31 UIOs are in this program and are at the forefront of diabetes care. Facilities use these funds to offer a wide range of diabetes treatment and prevention services, including but not limited to exercise programs and physical activity, nutrition services, community gardens, culinary education, physical education, health and wellness fairs, group exercise activities, green spaces, and youth and elder-focused activities.
The incredibly successful Special Diabetes Program for Indians (SDPI) has repeatedly been reauthorized in Continuing Resolutions and is now set to expire on March 14, 2025. We request that the committee work with authorizers to permanently reauthorize SDPI at a minimum of $250 million with automatic annual funding increases tied to the rate of medical inflation, to continue the success of preventing diabetes-related illnesses for all of Indian Country.
Request: Protect Medicaid and Authorize Permanent 100% Federal Medical Assistance Percentage for services provided at UIOs.
The Medicaid program plays a vital role in providing essential healthcare services to American Indian and Alaska Native communities, serving as a critical lifeline for those who rely on it. In fact, Medicaid is the largest source of funding for Urban Indian Organizations (UIOs) outside of the Indian Health Service (IHS). In 2021 alone, UIOs received over $137 million in Medicaid reimbursements for services delivered to Medicaid beneficiaries, underscoring the program’s significance in sustaining healthcare access for American Indian and Alaska Native populations.
NCUIH Board Vice President Angel Galvez recently emphasized the profound impact of Medicaid, stating, “The services we provide are services [our patients] can’t afford otherwise… What you’re doing is saving someone’s life.” 7 This sentiment highlights the life-saving role Medicaid plays in ensuring that vulnerable populations receive the care they need.
Protecting and strengthening the Medicaid program is essential to maintaining support for UIOs and the 59% of American Indian and Alaska Native patients they serve who depend on Medicaid for their healthcare. Safeguarding this program ensures that UIOs can continue to deliver critical services, ultimately improving health outcomes and quality of life for American Indian and Alaska Native communities.
A top Medicaid legislative priority for UIOs is providing 100% federal medical assistance percentage (FMAP) for services provided at UIOs. The FMAP refers to the percentage of Medicaid costs covered by the federal government and reimbursed to states. States have received 100% FMAP for services provided to IHS/Medicaid beneficiaries at Indian Health Service and Tribal facilities for decades, and UIOs have advocated for parity through legislation since 1999. Extending 100% FMAP to UIOs will require the federal government, not states, to bear the cost of Medicaid services provided to AI/AN people no matter which facet of the Indian health system they utilize, as is required by the trust responsibility.
Ultimately, permanent 100% FMAP will bring fairness to the I/T/U system and increase available financial resources to UIOs and support them in addressing critical health needs of urban American Indian and Alaska Native patients.
Request: Allow U.S. Public Health Service Commissioned Officers detailed directly to UIOs
Due to chronic underfunding, many UIOs continue to grapple with hiring and retaining skilled health service providers. Detailing Public Health Service Commissioned Officers (PHSCOs) to UIOs would help address workforce shortages and increase collaboration across the federal healthcare system.
Section 215 of the Public Health Service Act (PHSA) authorizes the Secretary of Health and Human Services (HHS) to detail officers to federal agencies and state health or mental health authorities. While UIOs have requested that officers be detailed to them to fill many roles related to the functions of the Public Health Service, subsection (c) of Section 215 (42 U.S.C. 215(c)) prevents UIOs from receiving detailed officers because they do not fall within the requirement that non-profits eligible for detailing be educational or research non-profits, or non-profits “engaged in health activities for special studies and dissemination of information”.
With this being said, subsection (b) has been interpreted to allow HHS to detail an officer to a state health authority, which may then designate the UIO as the officer’s duty station. The officer is authorized to perform work at a UIO that is related to the functions of the Service, including health care services and support functions. This process is completely dependent on the availability of a State or local health authority that is capable and willing to enter into such an arrangement. The process can be burdensome and time-consuming for all involved, leaving many State health authorities reluctant to participate.
Amending the law would provide IHS with the discretionary authority to detail officers directly to a UIO to perform work related to the functions of the Service. Therefore, we request full support for this proposal to allow UIOs to continue engaging in critical health care services for urban American Indian and Alaska Native communities.
Request: Fund the Initiative for Improving Native American Cancer Outcomes at $10 million for FY26
Rising cancer rates has become an increasingly alarming issue in Indian Country. In fact, cancer is the leading cause of death among American Indian and Alaska Native women and the second leading cause of death among American Indian and Alaska Native men.8 The rising cancer rates has been described by some UIO leaders as the “new diabetes” in Indian Country, with one clinic alone diagnosing 15-20 cases a month.
This is why specific funding for cancer in Indian Country is critical. The FY24 LHHS spending bill appropriated $6 million in few funding to address American Indian and Alaska Native cancer outcomes, by creating the Initiative for Improving Native American Cancer Outcomes, the Initiative will support efforts including research, education, outreach, and clinical access to improve the screening, diagnosis, and treatment of cancers among American Indian and Alaska Native people. The purpose of this Initiative is to ultimately improve screening, diagnosis and treatment of cancer for American Indian and Alaska Native patients.
This initiative will be critical to addressing cancer-related health disparities in Indian Country. We request that the Committee continue to support the appropriation of funds for the Initiative in FY26 and increase funding to $10 million.
Conclusion
These requests are essential to ensure that urban Indians are appropriately cared for, in the present and in future generations. The federal government must continue to work towards its trust and treaty obligation to maintain and improve the health of American Indians and Alaska Natives. We urge Congress to take this obligation seriously and provide the I/T/U system with all the resources necessary to protect the lives of the entirety of the American Indian and Alaska Native population, regardless of where they live.
[1] Relocation, National Council for Urban Indian Health, 2018. 2018_0519_Relocation.pdf(Shared)- Adobe cloud storage
[2] 25 U.S.C. § 1601(1)
[3] Contract Support Costs and Sequestration: Fiscal Crisis in Indian Country: Hearings before the Senate Committee on Indian Affairs.(2013) (Testimony of The Honorable Yvette Roubideaux)
[6] The Special Diabetes Program for Indians: Estimates of Medicare Savings, DHHS ASPE Issue Brief (May 10, 2019). Available at: SDPI_Paper_Final.pdf (hhs.gov)
[8] Elizabeth Arias, Kenneth Kochanek, & Farida B Ahmad, Provisional Life Expectancy Estimates for 2021, Vital Statistics Rapid Release, Report 23, August 2022. Vital Statistics Rapid Release, Number 023 (August 2022) (cdc.gov)