July Policy Updates: Interior Bill & IHS Funding, Supreme Court Updates, and Important Dates
Welcome to the July edition of our monthly policy newsletter, delivering the latest updates and insights on key developments.
1 Big Thing: House Advances Interior Bill with Advance Appropriations and a Modest Increase for Indian Health Service
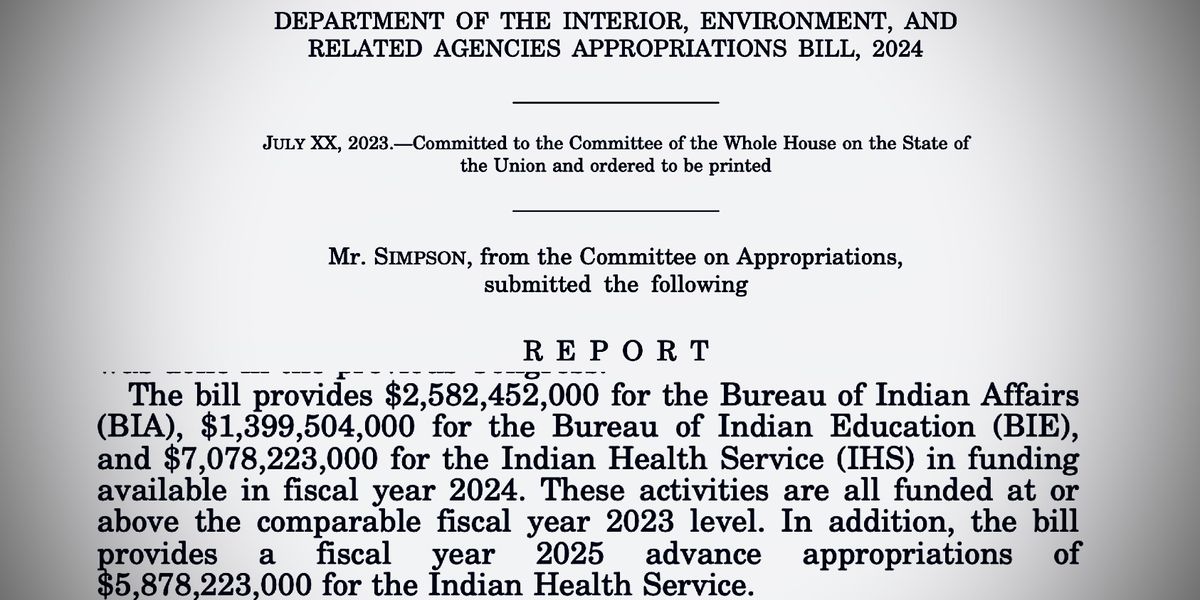
On July 18, 2023, the House Appropriations Subcommittee on Interior, Environment, and Related Agencies released the Committee Bill Report for the fiscal year (FY) 2024 budget.
- IHS Funding: The bill would authorize $7.078 billion for the IHS for FY24. That’s $149.4 million of the FY23 enacted level.
- Advance Appropriations: The bill also provides $5.878 billion in advance appropriations for FY 2025.
- Urban Indian Health: Includes the President’s proposed amount of $115.156 million for urban Indian health for FY24.
- CSC and Tribal Leases: The Subcommittee rejected the administration’s proposal and Tribal requests to make contract support costs and Tribal leases mandatory spending.
- The full Committee held a markup on July 19 and approved the FY 2024 Interior appropriations bill by a vote of 33 to 27.
What they’re saying: Rep. Mike Simpson (R-ID-2) on the Interior Markup:
“I am pleased that the bill provides a fiscal year 2025 advance appropriation for the Indian Health Service and it’s very important that we do that. I made a commitment from the start of this that we were not going to balance this budget on the backs of our Indian brothers and sisters, and we kept that commitment in this bill. It is a bipartisan commitment. We have a moral and a trust responsibility to the Indians of this country, and we need to make sure that we are trying to address that. We still have a long way to go, but we are moving in the right direction.”
What’s next: The bill has now passed out of committee and referred to the House floor. The Senate will be marking up the Interior Appropriations bill on July 27 at 10:30 a.m.
Go deeper:
Partnership and Advocacy: Tribal Sovereignty Payments for FY 2024

On July 12, 2023, NCUIH joined the National Indian Health Board (NIHB) and 21 Tribal Nations and Native partner organizations in sending a letter to House and Senate leadership regarding the Administration’s proposed FY 2024 Interior, Environment, and Related Agencies Appropriations Bill. The letter expresses support for the President’s FY 2024 proposal to reclassify Contract Support Costs and Section 105(l) Tribal Lease Payments as mandatory appropriations and to increase program administration staff. The letter also urges Congress to include the proposal in their FY 2024 Interior bill.
Supreme Court Updates

Department of Interior v. Navajo Nation
- On June 22, the Court held in a 5-4 decision that while the treaty establishing the Navajo Reservation reserved the necessary water to accomplish the purpose of the Navajo Reservation, it did not require the United States to take affirmative steps to secure water for the Tribe.
- This means that the government does not have an enforceable trust responsibility to secure water for the Tribe under the Treaty.
- Relation to UIOs: This holding further limits the scope of the enforceability of the trust responsibility.
Upcoming SCOTUS Cases for the 2023 term:
Loper Bright Enterprises v. Raimondo
- Case out of the D.C. Circuit, granted cert by SCOTUS in April.
- This case centers around whether a foundational case in Administrative Law, Chevron v. Natural Resources Defense Council, should be overruled. Under Chevron, a court must defer to a federal agency’s interpretation of an ambiguous statute so long as the agency’s interpretation is reasonable.
- If Chevron were to be overruled, federal agencies will be much more vulnerable to lawsuits for statutory interpretations as courts would no longer have to defer to an agency’s “reasonable” interpretation. This could cause a patchwork of enforceability for agency actions across circuits depending on the judicial interpretation.
- Relation to UIOs: If the Court decides to overrule Chevron, it would likely affect federal policies and programs and how federal agencies interact with UIOs regarding such policies and programs.
United States v. Rahimi
- Case out of the 5th. Circuit, granted cert by SCOTUS in June.
- This case centers around whether a federal law that prohibits the possession of firearms by persons subject to domestic violence restraining orders violates the Second Amendment.
- Relation to UIOs: If the Court determines that the law does violate the second amendment, it could loosen protections for persons who have filed domestic violence restraining orders in certain jurisdictions. This could potentially have an effect on UIO domestic violence work as well as work relating to Missing and Murdered Indigenous Peoples.
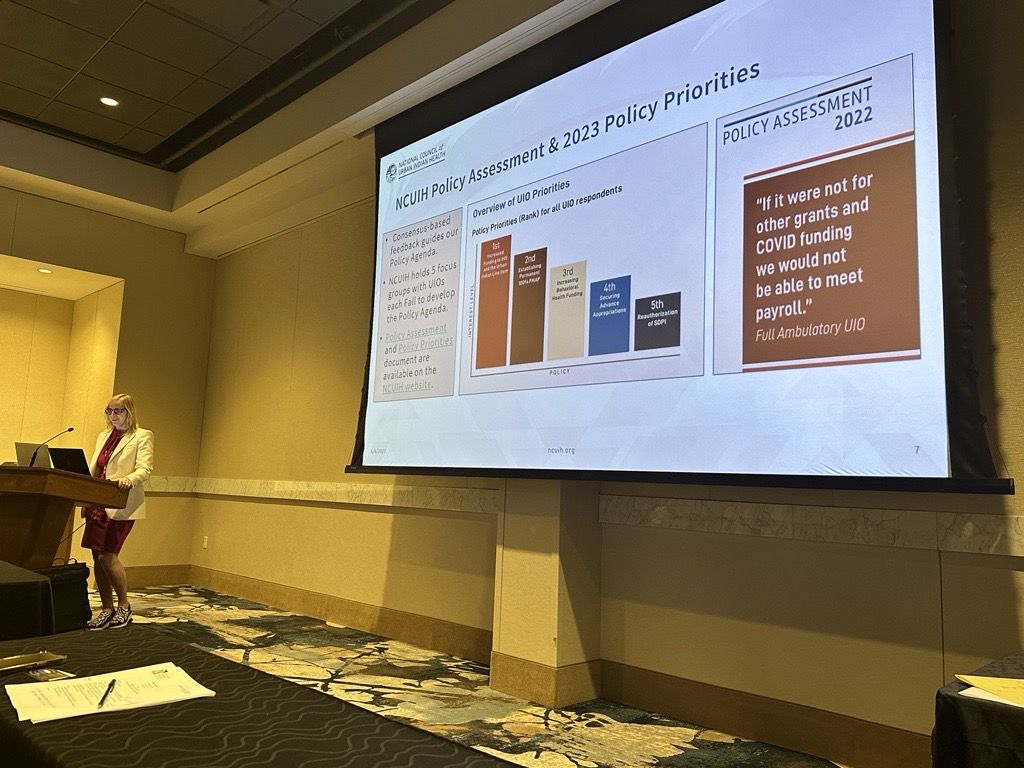
NCUIH Provides Comments on IHS Mandatory Funding & Access to Medicaid

On June 30, NCUIH submitted comments to the Office of Management and Budget (OMB) in support of IHS Mandatory Funding.
On July 3, NCUIH submitted comments to the Centers for Medicaid and Medicare Services (CMS) on Ensuring Access to Medicaid.
Our thought bubble: NCUIH recommended that CMS take the following actions:
- Ensure AI/AN representation on each state Medicaid Advisory Committee (MAC) and Beneficiary Advisory Group (BAG).
- Ensure the rule does not impose additional burdensome reporting requirements on providers.
- Engage with the Tribal Technical Advisory Committee (TTAG) to consider regulations or guidance to enforce the state consultation and confer requirements.
- Support 100% Federal Medical Assistance Percentage (FMAP) for Medicaid services provided at UIOs to ensure AI/AN Medicaid beneficiaries receive appropriate, quality culturally competent care.
Upcoming Comments and Submissions:
- August 21 – Comment deadline to the Department of Veterans Affairs (VA) Request for Data Information on Minority Veterans.
NCUIH Research Project Update
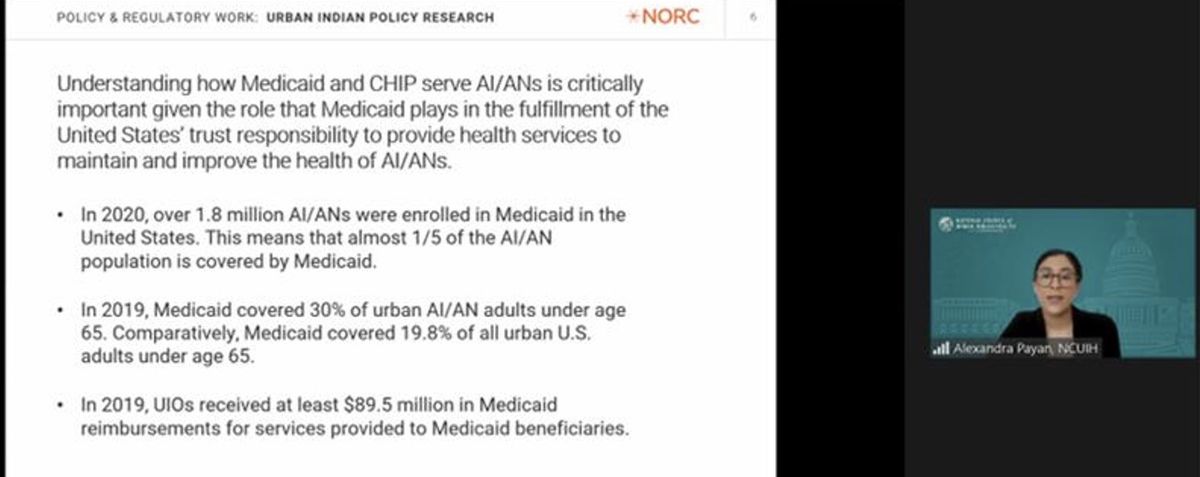
NCUIH Federal Relations Manager Alexandra Payan and Research Associate Nahla Holland gave updates to CMS Office of Minority Health on NCUIH’s NORC reports and research on PCCM programs/IMCEs and traditional healthcare practices at UIOs.
NCUIH is currently participating in its third year of a research project commissioned by CMS through a contract with NORC at the University of Chicago.
This year’s report provides an analysis of two topics:
- Primary Care Case Management (PCCMs) and Indian Managed Care Entities (IMCEs)
- Traditional Health Care Practices
What’s next: CMS has invited NCUIH to present the report findings during the July 2023 in-person TTAG meeting in Washington DC.
Upcoming Events and Important Dates
Upcoming Opportunities:
- The VA Office of Tribal Government Relations (OTGR), is seeking nominations of qualified candidates to be considered for appointment as a member of the Advisory Committee on Tribal and Indian Affairs (“the Committee”) to represent the following IHS Areas: Bemidji; California; Great Plains; Nashville; Navajo; Tucson. Nominations for membership on the Committee must be received no later than 5:00 PM Eastern on August 1, 2023, and should be mailed to OTGR at 810 Vermont Ave. NW, Suite 915H (075) or emailed to tribalgovernmentconsultation@va.gov. Individuals interested in participating in this Committee and who are located in the open IHS areas should work with local Tribes and tribal organizations to be nominated.
- The VA extended eligibility for VA health care for certain Veterans of the Vietnam, Gulf War, and post-9/11 eras pursuant to the Sergeant First Class Heath Robinson Honoring Our Promise to Address Comprehensive Toxics (PACT) Act. SUBMIT your PACT Act claim by August 9 to be eligible for backdated benefits back to August 10, 2022.
- On June 29, 2023, IHS Director Roselyn Tso released a Dear Tribal Leader Letter and Dear Urban Indian Organization Leader Letter giving an update on the IHS Health Information Technology (HIT) Modernization by sharing an opportunity for interested Tribal and UIOs sites to become directly involved in the collaborative planning for the new IHS enterprise electronic health record (EHR) solution. Interested UIOs are encouraged to complete and submit a Statement of Interest form by e-mail to modernization@ihs.gov and cc Policy@ncuih.org. There is no deadline for submitting the form.
Upcoming Events:
- July 20- Medicare, Medicaid, and Health Reform Policy Committee (MMPC) Regulations Workgroup Meeting
- July 25- MMPC Face-to-Face Prep Session for TTAG Meeting (in-person)
- July 26-27- CMS TTAG Face-to-Face Meeting (in-person)
- July 27- IHS Urban Program Executive Directors/Chief Executive Officers Monthly Conference Call
- August 1- NCUIH Board of Directors Meeting
- August 2- Tribal Consultation/Urban Confer: Health IT Modernization Leaders Engaging in Governance
- August 2-3- Not Invisible Act Commission National Virtual Hearing
- August 3- MMPC Regulations Workgroup Meeting
- August 16- FY25-FY26 Tribal Budget Formulation Planning and Evaluation Meeting (Hybrid)
ICYMI:
On June 20-21, IHS National Tribal Advisory Committee (NTAC) on Behavioral Health led a meeting:
- Dr. Segay, Director of the Division of Behavioral Health (DBH), noted that sections of the Indian Health Manual are being updated, specifically in sections focused on mental and behavioral health.
On June 30, CMS held a meeting with TTAG and STAC regarding the Four Walls Fix:
- CMS is considering revising its clinical regulations to tackle the Four Walls limitation, with the grace period for providing services outside of the clinic extended until Feb. 2025, but there are no guarantees regarding the outcomes as it may not be achievable through regulation.
On July 11, IHS held a meeting on the Overview of the Updated Policy on Conferring with UIOs:
- IHS will prepare a report to the UIOs with confer satisfaction results. The IHS will document and follow up on any unresolved issues that would benefit from the ongoing involvement of the affected UIO upon the completion of any of the conferring activities.
- Documentation of the conferring process and outcome will be maintained by the Office of Urban Indian Health Programs Headquarters office and area offices in which the affected UIOs are located.
On July 13, IHS held a July Tribal and UIO Leaders Call:
- The next Tribal and UIO leader call is set for August 3, 2023, and the 2023 IHS Partnership Conference will take place in Atlanta, GA, from August 22-24, 2023, with registration available until August 9th.
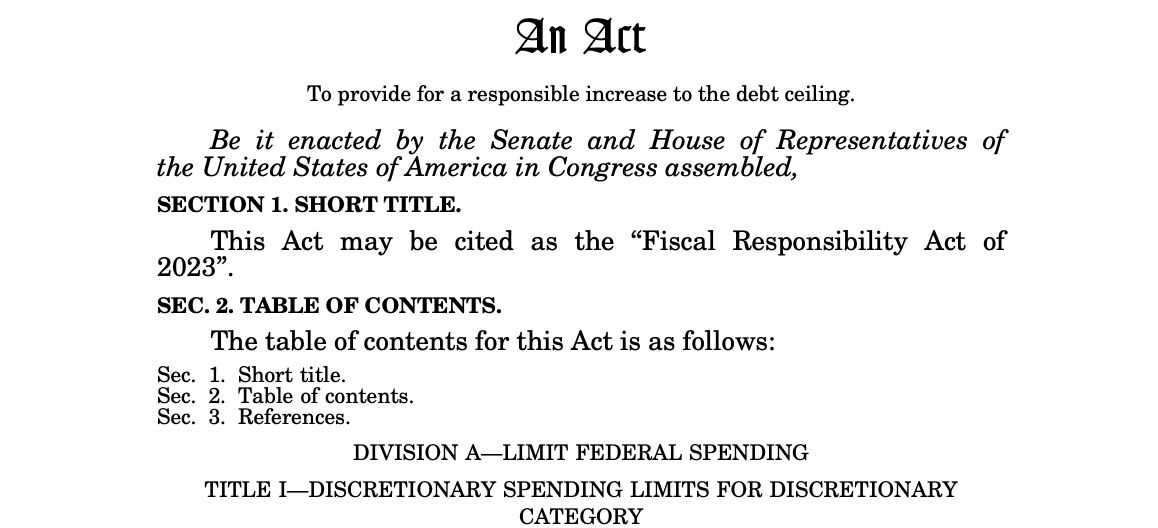
- There are also new Area Directors appointed, ongoing Covid-19 supplemental appropriations, and specific requirements outlined in the Fiscal Responsibility Act for FY 2024 and FY 2025 appropriations, including the need for Congress to pass full-year versions of all 12 appropriations bills by January 1, 2024.
Strengthening Relationships and Building Community at NCUIH

Senator Tester and NCUIH Summer Intern Tyler Rogers
On June 20, NCUIH attended the Poarch Band Creek Indians Legislative Reception.
Denver Indian Health and Family Services welcomes NCUIH!
NCUIH held its All Staff Retreat in Denver, Colorado from July 10-14 and staff visited the UIO, Denver Indian Health and Family Services.


NCUIH staff participate in a cultural wellness activity hosted by the Denver UIO.

NCUIH Staff Photo
NCUIH visits Red Rocks Park in Denver.
Thank you for all your hard work and advocacy!