Following Supreme Court Ruling, Support to Transition Contract Support Costs to Mandatory Appropriations Grows
On June 21, 2024, the National Council of Urban Indian Health (NCUIH), in partnership with the National Indian Health Board, National Congress of American Indians, and 25 other organizations, sent a letter urging Congressional Appropriations leaders to transition Contract Support Cost and 105(l) leases to mandatory appropriations. For over a decade, there has been significant pressure on Appropriators to transition Contract Support Costs to mandatory funding. In fact, in Fiscal Year (FY) 2014, the House and Senate Committees on Appropriations published a bipartisan, bicameral statement recognizing the mandatory nature and rapid growth of legally obligated Contract Support Costs (CSC) and expressing concern about the potential impact on the Interior bill. Since FY22, and included in FY25, the President’s budget has made a proposal to reclassify CSC and 105(l) payments as mandatory.
Federal and Congressional Support for Shifting CSCs and 105 (L) Leases to Mandatory Funding
Public statements by Department of Health and Human Services Secretary Becerra and Indian Health Service Director Tso urged “Congress to act on the FY 2025 President’s Budget proposal to shift the IHS budget from discretionary to mandatory funding starting in FY 2026 to protect the overall appropriation for the Indian Health Service and create more adequate and stable funding into the future”
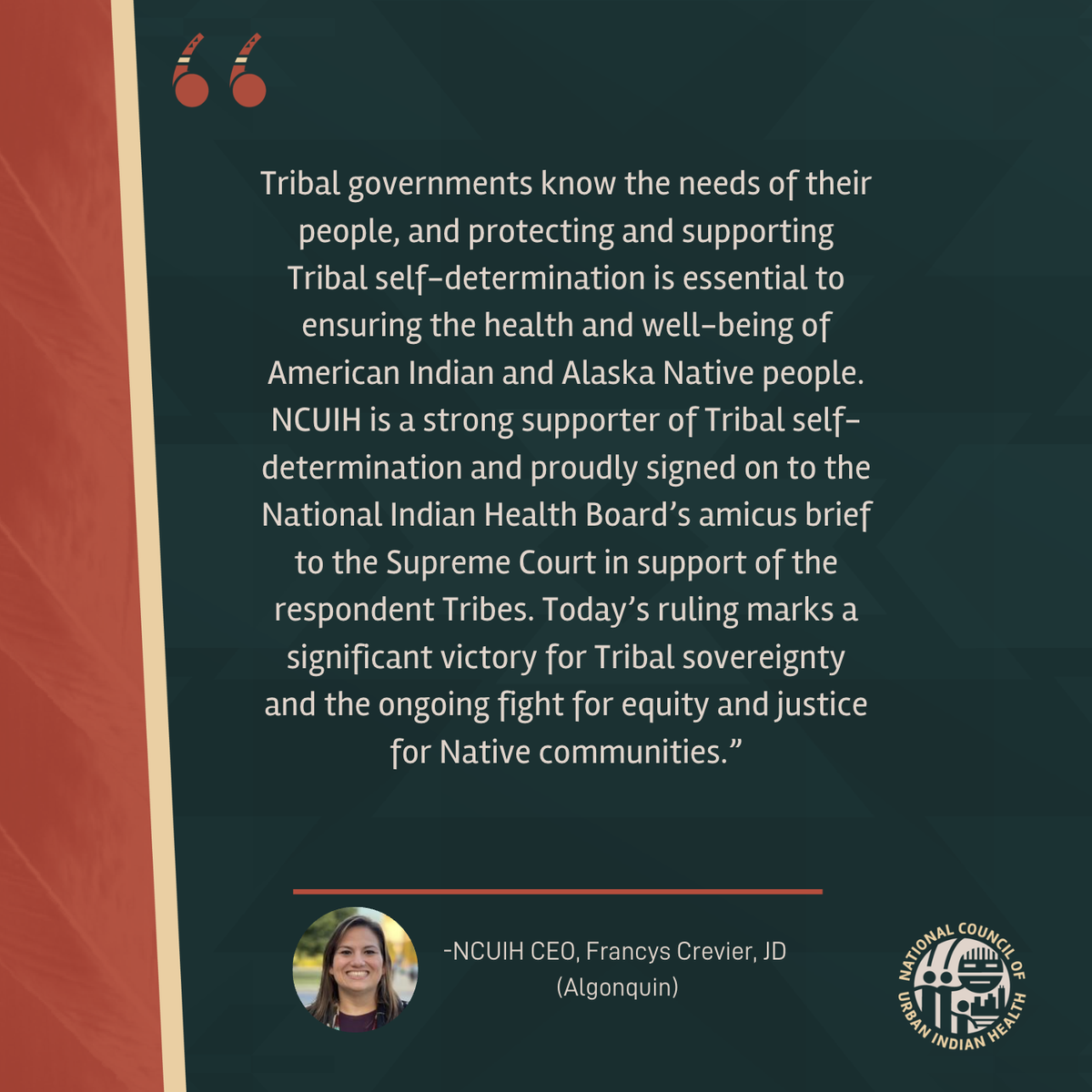
Following the June 6, 2024, Supreme Court’s opinion in favor of Tribes in the Becerra v. San Carlos Apache case, several House Appropriators called for shifting Contract Support Costs and Section 105(l) Tribal Lease Payments as mandatory appropriations. House Appropriations Chair Tom Cole stated that additional Indian Health Service spending will be needed after the Supreme Court decision. He also emphasized that the shift to mandatory appropriations, while it might take time, will be essential to continue funding the Indian Health Service and Urban Indian Health.
For more information on the Supreme Court ruling, check out NCUIH’s policy update and FAQ.
Full Text of the Letter:
Re: Support for the President’s FY25 Proposal for Mandatory CSC and 105(l) Funding
Dear Chair Murray, Chair Cole, Vice Chair Collins, and Ranking Member DeLauro:
On behalf of the undersigned Tribal partner organizations and our members, we strongly support the proposal to reclassify Contract Support Costs and Section 105(l) Tribal Lease Payments as mandatory appropriations. We respectfully urge you to include the proposal in the FY25 Interior and Environment Appropriations bill (hereinafter “Interior bill”). The President’s budget request has consistently recommended this change since FY 2022.
Ten years ago, for FY14, the House and Senate Committees on Appropriations (hereinafter “Committees”) published a bipartisan, bicameral statement recognizing the mandatory nature and rapid growth of legally obligated Contract Support Costs (CSC) and expressing concern about the potential impact on the Interior bill. They stated:
“[T]he House and Senate Committees on Appropriations are in the untenable position of appropriating discretionary funds for the payment of any legally obligated contract support costs. Typically obligations of this nature are addressed through mandatory spending, but in this case since they fall under discretionary spending, they have the potential to impact all other programs funded under the Interior and Environment Appropriations bill, including other equally important tribal programs.”
Six years later, for FY20, the Committees published a similar statement regarding payments related to Tribal Lease Payments required by Section 105(l) of the Indian Self-Determination and Education Assistance Act (hereinafter “105(l) payments”.) The Committees expressed concern that 105(l) payments “are negatively impacting the ability to use discretionary appropriations to support core tribal programs, including health, education and construction programs, or provide essential fixed cost requirements.” The Committees called on the Department of the Interior and the Department of Health and Human Services (HHS) to “formulate long-term accounting, budget, and legislative strategies to address the situation, including discussions about whether, in light of the Maniilaq decisions, these funds should be re-classified as an appropriated entitlement.” Since FY22, the Departments of the Interior and HHS have requested that CSC and 105(l) payments be appropriated as mandatory, but Congress has not yet acted on this common-sense proposal.
After the Committees highlighted the problem in FY20, the Interior bill has continued to struggle to simultaneously address historically underfunded Tribal programs while keeping up with the growth of CSC and 105(l) payments. In FY24, appropriations for CSC and 105(l) payments increased by $168 million (12%). However, these increases were offset by cuts to other Tribal programs in the Indian Health Service (IHS) and the Bureaus of Indian Affairs and Education. In all, the agencies received a combined $23 million topline cut and were denied the $421 million requested for fixed costs, inflation, and population growth to simply maintain current levels of service. FY25 is shaping up to be an even bigger challenge, with CSC and 105(l) payments estimated to increase by another $268 million (17%).
On June 6, 2024, the U.S. Supreme Court ruled that the IHS must pay contract support costs on revenue collected from 3rd party payers like Medicare, Medicaid, and private insurance. This will undoubtedly have major budget implications for the IHS CSC budget on top of the annual increases impacting the budget. The government argued that this decision could cost up to $2 billion annually, which would more than double the current CSC obligation. With the Fiscal Responsibility Act in place, domestic discretionary spending will increase by just 1%. This is not nearly enough to absorb these costs without further cuts to other essential services and programs. Now is the time to reclassify these costs appropriately, as mandatory funding.
Simply put, both programs will continue to grow as they continue to be utilized by Tribal nations throughout the United States, and the Interior bill will continue to fail to meet its trust and treaty obligations to Tribes under the budget structure and process currently in place. Reclassifying CSC and 105(l) payments as mandatory would be a positive step and would be consistent with budgeting for most other Federal legal obligations where full and timely payments minimize litigation risk. Moreover, as with other recently reclassified mandatory appropriations in the Interior bill, the Committees could retain oversight of the programs.
The President’s FY25 proposal to reclassify CSC and 105(l) payments as mandatory is reasonable, fair, and a direct response to the Committee’s bipartisan, bicameral calls for a long-term solution. Our organizations recognize and appreciate your strong leadership and bipartisan support over the years for Tribal self-determination. For the sake of continuing to improve the federal government’s commitments to meeting its trust and treaty obligations under your leadership, we urge you to include the President’s proposal in the FY25 Interior bill.
Sincerely,
National Indian Health Board
National Congress of American Indians
Self-Governance Communication and Education Tribal Consortium
National Council of Urban Indian Health
Alaska Federation of Natives
Alaska Native Health Board
Albuquerque Area Indian Health Board
Association of American Indian Physicians
Affiliated Tribes of Northwest Indians
United South and Eastern Tribes Sovereignty Protection Fund
Rocky Mountain Tribal Leaders Council
Seattle Indian Health Board
Rocky Mountain Tribal Leaders Council
Northwest Portland Area Indian Health Board
Great Lakes Area Tribal Health Board
Inter-Tribal Association of Arizona
California Rural Indian Health Board
California Tribal Chairmans Association
Coalition of Large Tribes
Southern Plains Tribal Health Board
Great Plains Tribal Leaders Health Board
Midwest Alliance of Sovereign Tribes
American Indian Higher Education Consortium
National American Indian Housing Council
National Indian Education Association
National Indian Child Welfare Association
National Native American Boarding School Healing Coalition
Navajo Nation