House Passes NCUIH-Endorsed Bipartisan Bill that Improves Home and Community-Based Services for Native Veterans, Includes Collaboration with Tribal Programs and Urban Indian Organizations
On December 5, 2023, the House passed the National Council of Urban Indian Health (NCUIH)-endorsed legislation, the Elizabeth Dole Home-and Community-Based Services for Veterans and Caregivers Act of 2023 (H.R. 542) with a vote of 414-5. The bill has now been received in the Senate. The original sponsor, Rep. Julia Brownley (D-CA-26) reintroduced this bipartisan legislation on January 26, 2023, which would direct the Department of Veterans Affairs (VA) to expand options for long-term home and community services. The bill also directs the VA to collaborate with the Director of the Indian Health Service (IHS) and representatives from tribal health programs and Urban Indian Organizations (UIOs) to ensure the availability of home-and community-based services for Native American veterans, including Native American veterans receiving health care and medical services under multiple health care systems. The bill currently has 63 Democrat and 13 Republican co-sponsors.
Specifically, the bill expands existing Home and Community Based Services (HCBS):
- The Veteran Directed Care Program, which provides veterans a flexible budget to hire friends, family, and neighbors to help with activities of daily living, such as bathing, or instrumental activities of daily living, such as making meals.
- The bill directs the VA Secretary to ensure the availability of the program for eligible veterans who are Native American veterans receiving care and services furnished by the Indian Health Service, a tribal health program, an Urban Indian organization, or (in the case of a Native Hawaiian veteran) a Native Hawaiian health care system, to the extent practicable.
- The Homemaker and Home Health Aide Program, which allows VA to contract with a community partner that employs home health aides to care for veterans in their homes, providing skilled services, case management, help with daily living, or to ease caregiver burnout.
- The Home-Based Primary Care Program, which allows for a VA physician to supervise a health care team that provides care in the veteran’s home for a veteran who has difficulty traveling or is isolated.
- The Skilled Home Health Care Program, which allows for VA to contract with a community health agency to provide in-home care for veterans who have higher levels of need like wound care, speech therapy, or skilled nursing.
“Every veteran should have the right to a peaceful and dignified life after their service to our country, and every veteran should have the right to stay in their home and receive the care they need, the care they have earned, and the care they deserve.” – Congresswoman Julia Brownley (D-CA)
Background on Native Veterans
Native Veteran Disparities
Native veterans have served in the United States military in every armed conflict in the Nation’s history and have traditionally served at a higher rate than any other population in the United States. Unfortunately, Native veterans suffer significant disparities when they transition to civilian life. For example, Native veterans are more likely to be uninsured and have a service-connected disability than other veterans. Native veterans suffer these disparities no matter where they live. Native veterans living in urban areas experience the same poor physical and mental health outcomes as Native veterans in rural areas. In addition, urban Native veterans generally have lower incomes, higher unemployment, lower education attainment, higher VA-service connected disability, and generally live in poorer housing conditions than non-Native urban veterans.
Urban Indian Organizations Provide Culturally Competent Care for Native Veterans
UIOs are essential partners in serving Native veterans and are vital to improve care and access to services for Native veterans because of their deep ties to the Native community in urban areas. UIOs currently serve seven of the ten urban areas with the largest Native veteran populations, including the following areas: Phoenix, Arizona; Los Angeles, California; Seattle, Washington; Dallas, Texas; Oklahoma City, Oklahoma; New York City, New York; and Chicago, Illinois.
UIOs are uniquely positioned to assist the VA in improving culturally competent healthcare access for Native people. As such, this partnership has the potential to improve the quality of care and well-being to Native veterans in urban areas, but it is also consistent with the United States’ trust responsibility to provide services and resources to improve the health of all Native people.
Next Steps
This bill has been received in the Senate. NCUIH will continue to monitor the bill’s progress.



 The National Council of Urban Indian Health (NCUIH) is pleased to announce the release of its
The National Council of Urban Indian Health (NCUIH) is pleased to announce the release of its 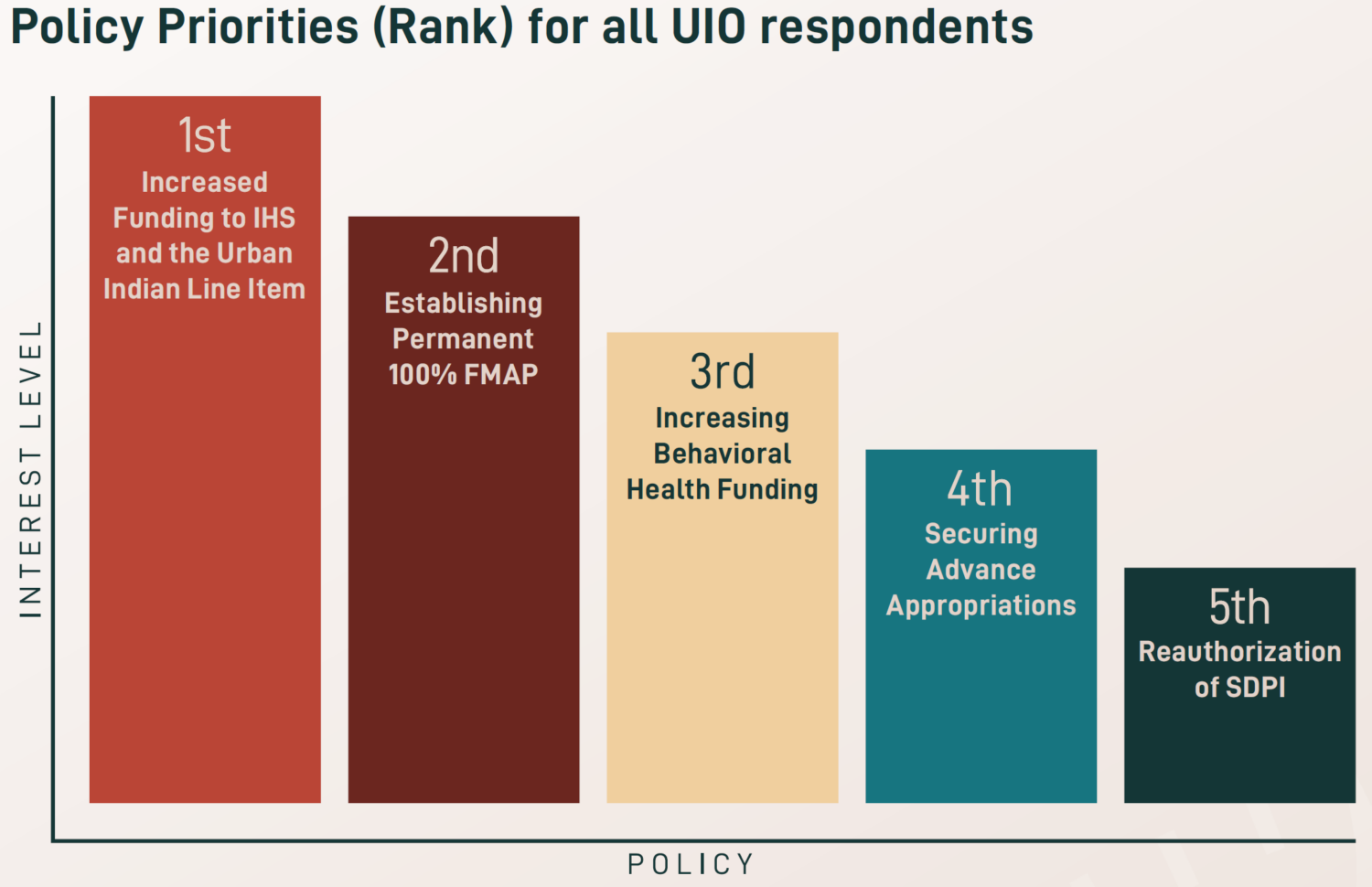 After the height of the COVID-19 pandemic, newfound priorities were identified for 2023, including workforce development and retention, increased funding for traditional healing, and expanded access to care and telehealth services. Existing priorities also remain a key focus across UIOs, especially increasing funding amounts for the urban Indian health line item and IHS, maintaining advance appropriations for IHS, establishing permanent 100% Federal Medical Assistance Percentage (FMAP) for UIOs, reauthorizing the Special Diabetes Program for Indians (SDPI), and increasing behavioral health funding.
After the height of the COVID-19 pandemic, newfound priorities were identified for 2023, including workforce development and retention, increased funding for traditional healing, and expanded access to care and telehealth services. Existing priorities also remain a key focus across UIOs, especially increasing funding amounts for the urban Indian health line item and IHS, maintaining advance appropriations for IHS, establishing permanent 100% Federal Medical Assistance Percentage (FMAP) for UIOs, reauthorizing the Special Diabetes Program for Indians (SDPI), and increasing behavioral health funding.