Senate Committee on Indian Affairs Passes NCUIH Endorsed Truth and Healing on Indian Boarding School Policies Act
On June 7, 2023, the Senate Committee on Indian Affairs (SCIA) held a business meeting where they unanimously passed the National Council of Urban Indian Health (NCUIH)-endorsed legislation, the Truth and Healing Commission on Indian Boarding School Policies Act (S.1723) with amendments. This legislation establishes a formal commission to investigate, document, and acknowledge past injustices of the federal government’s Indian Boarding School Policies. The Commission would develop recommendations for Congress to promote the healing of historical and intergenerational trauma caused by boarding schools and provide an environment for American Indian/Alaska Native (AI/AN) people to speak about their personal experiences.
SCIA Chairman, Senator Schatz (D-HI), highlighted that “for over a century, the federal government knowingly perpetuated violence and trauma with the goal of assimilating Native children by destroying family and communal bonds, their languages, their cultures, and their very identities. The impacts of this shameful history are felt by survivors and their descendants to this day. Without the guidance and support of Native communities across the country on this important bill, a culturally respectful and meaningful path to truth and healing would not be possible.”
SCIA Vice Chairman, Senator Murkowski (R-AL), echoed the importance of the legislation, stating, “This Commission will help document what happened and then develop recommendations on how to heal from these harms. I commend the work of the committee staff and members for their efforts to address the calls for justice by advocates while making bipartisan improvements to the bill.”
The adopted amendments reflect feedback from over 100 survivors, descendants, Tribal leaders, advocates, churches, local governments, and experts, who provided testimony for the record following last year’s hearing. These amendments include requiring the online publication of final reporting, giving the Attorney General authority to prevent the issuance of a defective subpoena after providing the opportunity to cure, enabling the Commission to use data provided by the Department of the Interior to prevent duplication, clarifying that the Commission may not use federal funds to purchase property, requiring that subpoenas get a unanimous vote on the five-member Commission, and ensuring the commissioner is serving as the traditional cultural authority is recognized as such by their respective native community.
Re-Introduction of the Bill
This legislation was previously introduced by Congresswomen (now Secretary of Interior) Deb Haaland (D-NM) in 2020 as H.R. 8420 and Senator Elizabeth Warren and Representatives Sharice Davids (D-KS-03) and Tom Cole (R-OK-04) in 2021 as H.R. 5444/S.2907. On May 18, 2023, Senator Warren (D-MA) re-introduced the bill as S.1723 with bipartisan support and 26 co-sponsors.
The bill is endorsed by the National Native American Boarding School Healing Coalition (NABS), National Congress of American Indians (NCAI), National Indian Education Association (NIEA), National Indian Health Board (NIHB), National Indian Child Welfare Association (NICWA), American Indian Higher Education Consortium (AIHEC), National Indigenous Women’s Resource Center (NIWRC), Seattle Indian Health Board (SIHB), Jesuit Conference of Canada and the United States, Friends Committee on National Legislation (FNCL), and United South and Eastern Tribes Sovereignty Protection Fund (USET SPF).
Background
The federal government funded these boarding schools as recently as the 1960s to wipe out Indigenous cultures. Children were forcibly removed from their families and experienced horrific emotional, physical, and sexual abuse while in the custody of these schools. The Commission not only highlights the government’s role in the abuse but will also build on the work of Secretary Deb Haaland and the Department of the Interior in examining what happened at these schools.
On June 22, 2022, the Senate Committee on Indian Affairs held a hearing to consider Truth and Healing Commission on Indian Boarding School Policies in the United States Act, S. 2907 and on June 15, 2022, the House Committee on Natural Resources held a markup to consider a series of bills, including the House companion bill . Several Members of Congress, such as Senator Cortez Masto (D-NV) and Representative McCollum (D-MN-04), expressed concerns and grievances about the horrific occurrences within boarding schools.
On December 23, 2021, NCUIH submitted comments to the Department of the Interior regarding the agency’s Federal Boarding School Initiative, reiterating its ongoing support for the Administration’s efforts to address the legacy of boarding school programs while urging the Administration to use the Initiative to address the public health impact of boarding schools on urban AI/ANs.
NCUIH Action
NCUIH worked with Senator Elizabeth Warren (D-MA) on this landmark legislation to begin the healing process from Indian Boarding School policies and ensure the inclusion of urban Indian organizations in the Commission. This bill ensures that the stories of AI/ANs that live in urban areas are included. NCUIH exists partly because of the historical oppression of the AI/AN population, including federal boarding schools that resulted in the growing AI/AN populations in cities, and has continuously advocated for substantial efforts to address the historical trauma and public health impact that boarding schools have on urban AI/ANs.
On December 23, 2021, NCUIH submitted comments to the Department of the Interior regarding the agency’s Federal Boarding School Initiative, reiterating its ongoing support for the Administration’s efforts to address the legacy of boarding school programs while urging the Administration to use the Initiative to address the public health impact of boarding schools on urban AI/ANs.
On May 26, 2022, NCUIH submitted written testimony to the House Natural Resources Subcommittee for Indigenous Peoples of the United States in support of the Truth and Healing Commission on Indian Boarding School Policies in the United States Act (S. 2907/H.R. 5444).
Next Steps
This legislation has been read twice and referred to the Committee on Indian Affairs. NCUIH will continue to monitor the bill’s progress.
Resources
- Full Bill Text – S.1723
- Senator Warren Press Release on reintroduction of the bill
- NCUIH Endorsed Bill Introduced by Sen. Warren, Rep. Davids and Rep. Cole on National Day of Remembrance (October 15, 2021)
- NCUIH Submits Comments to DOI on Boarding School Initiative and the Lasting Impact on Urban Indian Health (December 23, 2021)
- House Advances NCUIH-Endorsed Truth and Healing Commission on Indian Boarding Schools Bill – NCUIH (June 24, 2022)

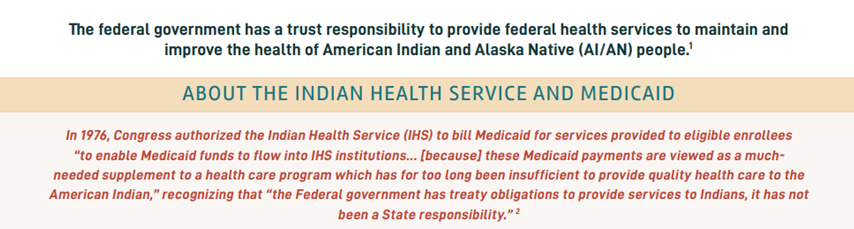
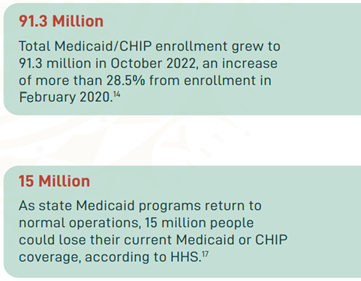 In March 2020, the Families First Coronavirus Response Act (FFCRA) Medicaid and Children’s Health Insurance Program (CHIP) “continuous coverage” requirement allowed people to retain Medicaid coverage and receive needed care during the COVID-19 Pandemic Public Health Emergency (PHE).
In March 2020, the Families First Coronavirus Response Act (FFCRA) Medicaid and Children’s Health Insurance Program (CHIP) “continuous coverage” requirement allowed people to retain Medicaid coverage and receive needed care during the COVID-19 Pandemic Public Health Emergency (PHE).