Commonwealth Fund’s 2023 Scorecard Reveals Alarming Disparities In Maternal Health For Native Communities Across The US
On July 22, 2023, the Commonwealth Fund released a Scorecard ranking every state’s health care system based on how well it provides high-quality, accessible, and equitable health care. The Commonwealth Fund’s 2023 Scorecard on State Health System Performance includes a new dimension focused on Reproductive Care and Women’s Health, which measures health outcomes and access to important services for women, mothers, and infants – including for American Indians and Alaska Natives (AI/ANs). The Scorecard reports high and increasing rates of maternal mortality, with AI/AN women facing the highest rates of maternal mortality during the pandemic. Due to barriers such as cost, discrimination, and lack of cultural competency, AI/AN communities throughout the country, including urban AI/AN communities, experience significant maternal and infant health disparities compared to the general population.
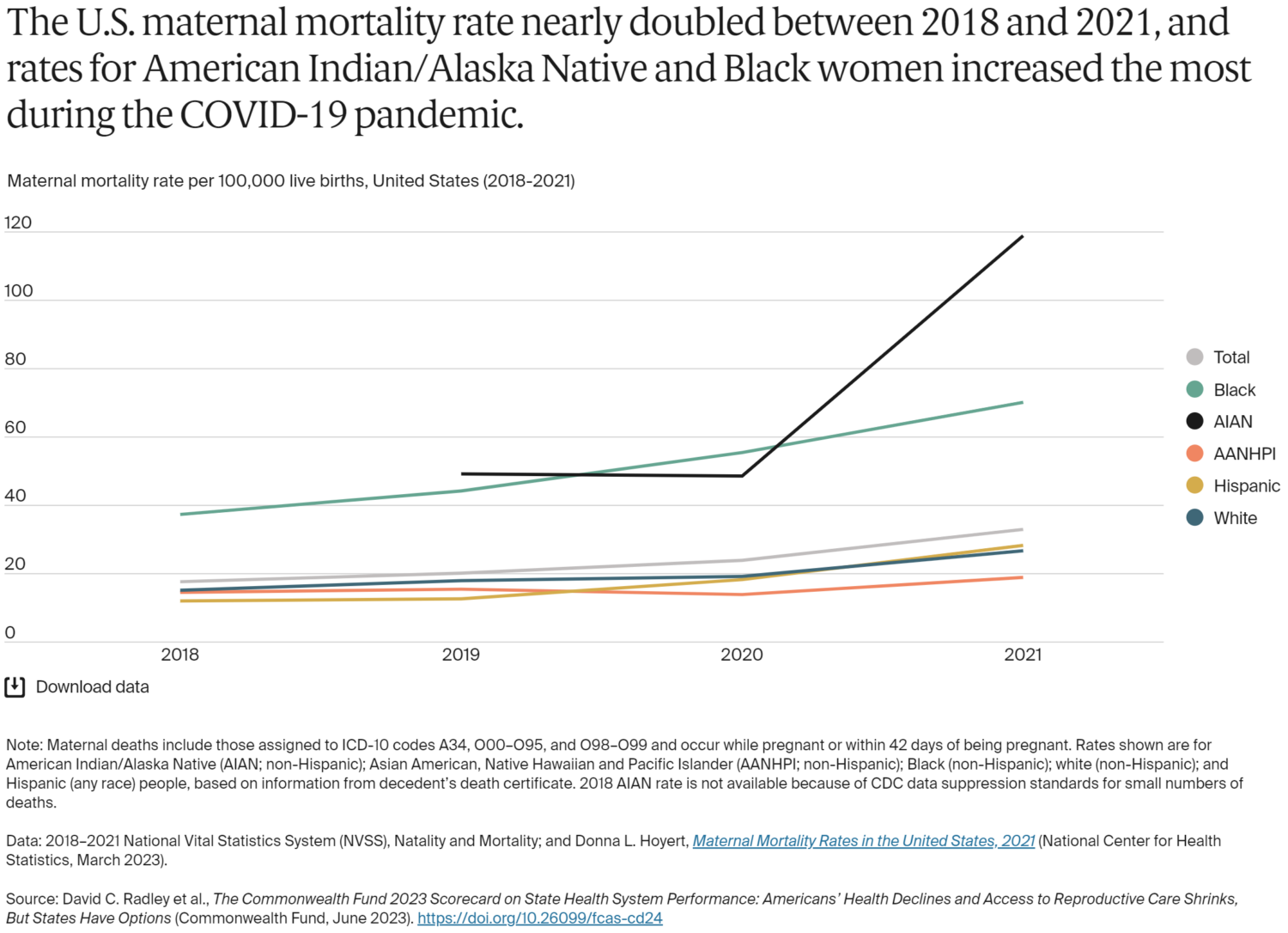
According to the Scorecard, the maternal death rate for AI/AN women jumped by nearly 70 deaths per 100,000 live births between 2019 and 2021, putting them well above other racial and ethnic groups. Among the likely causes were the greater burden of COVID-19 in AI/AN communities; higher rates of poverty, food insecurity, and other social risk factors; and disparities in insurance coverage and quality of care.
The convergence of the prolonged pandemic, existing maternal mortality crisis, and barriers to reproduce healthcare access, including the overturning of Roe v. Wade, poses significant challenges for women’s health, especially AI/AN women. Restrictive abortion laws and poor health outcomes are correlated, and there is concern that existing gaps in reproductive care may widen in the future. AI/AN women face challenges in accessing timely and affordable healthcare and are affected by the behavioral health crisis and the lingering effects of COVID-19.
AI/AN Maternal and Infant Health Disparities
According to the Office of Minority Health (OMH), Native infants have almost twice the infant mortality rate as non-Hispanic whites. Native infants are also almost three times more likely than non-Hispanic whites to die from accidental deaths before the age of one year. Contributing factors to these disparities include cost, discrimination, and lack of cultural competency during prenatal care. Additional ongoing and historical trauma due to colonization, genocide, forced migration, and cultural erasure also contribute to health inequities, including pregnancy-related deaths and other maternal health conditions. Approximately 41% of AI/AN women cite cost as a barrier to receiving the recommended number of prenatal visits and 23% of AI/ANs report they have faced discrimination in clinical settings due to being an AI/AN. Consequently, AI/AN people are more likely to have underlying chronic health conditions, and they face systemic barriers to care including higher rates of poverty and needing to travel long distances to receive quality health care services.
NCUIH and UIO Work on AI/AN Maternal and Infant Health.
UIOs provide a range of services such as primary care, behavioral health, traditional, and social services— including those for infants, children, and mothers. At least 23 of these clinics provide care for maternal health, infant health, prenatal, and/or family planning. They also provide pediatric services and participate in maternal-child care programs such as WIC and the Health Resources and Services Administration (HRSA) Maternal, Infant, and Early Childhood Home Visiting program (MIECHV).
The National Council of Urban Indian Health (NCUIH) has engaged in extensive advocacy on behalf of AI/AN mothers and infants and for increased funding and support to the UIOs which provide maternal health, infant health, prenatal, and family planning services to AI/AN mothers and infants. In March 2022, NCUIH signed onto a letter to Congress led by the National Home Visiting Coalition in support of reauthorizing HRSA’s MIECHV program and doubling the Tribal set-aside – which includes UIOs. Earlier this year, NCUIH submitted comments to the Administration for Children and Families (ACF) recommending that ACF ensure urban Native communities are participating in the Tribal MIECHV program by hosting an Urban Confer with UIO leaders to discuss the program and working with its colleagues at IHS to host and facilitate an Urban Confer on the annual reporting requirements. Additionally, in August 2022, NCUIH submitted comments to the HRSA Maternal and Child Health Bureau (MCHB) regarding the Pediatric Mental Health Care Access Program. In our comments, we have continued to stress the critical importance of including urban Native populations in HRSA’s overall efforts to improve health outcomes for all AI/ANs living on and off reservations.
NCUIH has also worked closely with HRSA’s Advisory Committee on Infant and Maternal Mortality (ACIMM) on AI/AN maternal and infant health issues. On September 14, 2022, NCUIH’s Vice President of Policy and Communications, Meredith Raimondi, testified before the HRSA ACIMM on urban Indian disparities and policy changes to address these disparities, and on December 7, 2022, the NCUIH provided recommendations to the ACIMM to ensure the needs of off-reservation AI/AN mothers were included in their report to the Department of Health and Human Services (HHS) Secretary Xavier Becerra titled: “Making Amends: Recommended Strategies and Actions to Improve the Health and Safety of American Indian and Alaska Native Mothers and Infants”.