Maximizing SDPI Impact: Effective Strategies and Data-Driven Solutions for UIOs
Background
Urban Indian Organizations (UIOs) play a vital role in addressing diabetes disparities within urban American Indian and Alaska Native (AI/AN) communities through the Indian Health Service’s (IHS) Special Diabetes Program for Indians (SDPI). Established by Congress in 1997, SDPI has been a cornerstone in diabetes prevention and treatment efforts, providing UIOs with critical funding to support culturally tailored health interventions. Over the years, SDPI has contributed to significant reductions in diabetes-related complications and has improved overall health outcomes within AI/AN communities (IHS SDPI Overview and Outcomes).
Through SDPI, UIOs have developed comprehensive programs integrating traditional healing practices with modern medical care, fostering a holistic approach to diabetes prevention and management. These efforts reduce the prevalence of diabetes-related complications and empower AI/AN individuals to take control of their health through education, early screening, and lifestyle support. Despite significant progress, UIOs continue to face challenges such as resource limitations, workforce shortages, and evolving patient needs. By refining strategies, leveraging data-driven solutions, and building supportive partnerships, UIOs can build upon their SDPI successes and drive even greater impact in urban AI/AN communities.
Comprehensive SDPI Services at UIOs
To better understand how UIOs are leveraging SDPI resources, NCUIH analyzed 2025 program profiles to identify the most commonly offered services across urban Indian health settings.
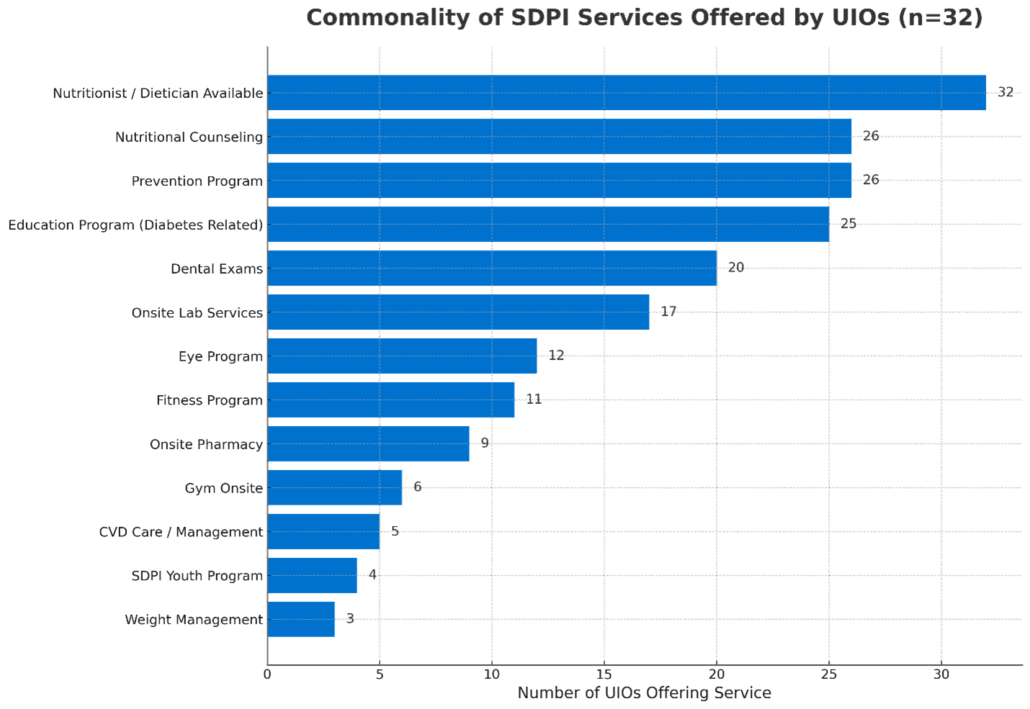
Figure 1. Commonality of SDPI Services Offered by UIOs (n=32)
Source: NCUIH Program Profiles, 2025. Data reflect the number of Urban Indian Organizations reporting each SDPI-related service.
SDPI-funded programs at UIOs offer a robust and holistic suite of services designed to meet the diverse needs of AI/AN communities. Among the most frequently provided offerings are diabetes-related education programs and blood glucose monitoring through onsite lab services, underscoring the importance of early detection and proactive treatment. Additionally, services such as access to a nutritionist or dietician, nutritional counseling, and prevention programs are critical components of both diabetes prevention and long-term disease management. UIOs also provide fitness programming and culturally relevant education initiatives that empower individuals to make informed health choices.
The success of these services highlights the commitment of UIOs to patient-centered care, where both traditional knowledge and evidence-based medicine work in tandem. Expanding access to specialized offerings, such as medication monitoring and long-term follow-ups, can further enhance health outcomes and ensure continued progress in diabetes prevention and management.
Enhancing Diabetes Program Performance
Performance metrics, guided by the Government Performance and Results Act (GPRA), highlight SDPI’s impact. Between 2018 and 2019, UIOs demonstrated improvements in blood pressure control rates, with the average rate increasing from 62.8% in 2018 to a peak of 64.2% in 2019[1]. Although external factors like the COVID-19 pandemic disrupted recent trends, UIOs quickly adapted by incorporating innovative solutions, including telehealth and at-home monitoring tools.
Success Story: Expanding Diabetes Care with Telehealth
At NATIVE HEALTH in Phoenix, a UIO-supported SDPI program successfully expanded its diabetes care services by integrating telehealth and remote patient monitoring. By distributing wireless glucose monitors and offering virtual diabetes education sessions, NATIVE HEALTH significantly improved patient engagement and glycemic control among its urban AI/AN population. This approach has since been adopted by other UIOs, demonstrating the effectiveness of digital tools in chronic disease management. Programs that consistently achieve high performance often incorporate robust case management and proactive outreach strategies, which can serve as models for other UIOs.
Strategies for Strengthening SDPI Services
To build on current successes and address identified challenges, UIOs can implement the following five strategic approaches:
- Expand Specialized Diabetes Care
- Increase access to medication monitoring, individualized dietary counseling, and comprehensive follow-up care.
- Leverage telehealth services to improve patient access to specialized diabetes care (IHS Telehealth Resources).
- Standardize Data Reporting
- Implement a universal service taxonomy to improve reporting accuracy and transparency.
- Utilize comprehensive electronic tracking systems to ensure consistent data collection and analysis through patient electronic health management systems.
- Staff Training and Development
- Conduct regular training to enhance accurate, standardized reporting practices (NCUIH Technical Assistance and Training).
- Designate dedicated data leads at each UIO to oversee reporting and ensure data integrity.
- Continuous Quality Improvement
- Perform routine data audits to identify strengths and opportunities for growth.
- Establish peer learning networks to facilitate knowledge-sharing and best practice adoption, such as participation in NCUIH Learning Collaboratives.
- Align Services with Performance Metrics
- Ensure service offerings align with GPRA performance metrics to maximize program impact.
- Use data visualization dashboards to track service provision and patient outcomes more effectively (IHS Quality Metrics).
Collaborative Partnerships
Collaboration is key to maximizing SDPI’s impact. UIOs are encouraged to actively engage with NCUIH, IHS, other UIOs, and SDPI technical assistance teams to enhance service delivery, improve data collection methods, and share successful strategies. Strengthening partnerships with local health care providers and community organizations can also support program sustainability and expand patient access to diabetes care services (NCUIH Partnership Resources).
Conclusion
Through SDPI support, UIOs continue to make meaningful progress in combating diabetes in urban AI/AN communities. By implementing evidence-based strategies and leveraging data-driven insights, UIOs can further enhance diabetes care, reduce disparities, and improve overall health outcomes. Continued collaboration and strategic investment are essential to sustaining these advancements and ensuring healthier futures for AI/AN populations in urban settings.
Need tailored data insights for your SDPI program? Contact our research team for support. Submit a Request for Data Support (Research – NCUIH).
[1]FY 2018 Urban GPRA Report_FINAL.pub.pdf; FY 2019 Urban GPRA Report_FINAL.pdf