Resource: An Overview of the Impact of Medicaid on Health Care of American Indians and Alaska Natives
The National Council of Urban Indian Health (NCUIH) recently released an infographic showcasing the impact of Medicaid on health care for American Indian and Alaska Native (AI/AN) people. This document highlights data and statistics on AI/AN Medicaid coverage and enrollment, the impact of Medicaid funding on Indian healthcare providers, information on COVID-19 and Medicaid unwinding, and how Medicaid affects Urban Indian Organizations (UIOs) and urban AI/ANs.
About the Indian Health Service and Medicaid
Medicaid is a joint federal-state program that provides health insurance to eligible persons, including eligible AI/ANs. Indian healthcare providers bill Medicaid for services provided to Medicaid beneficiaries and Medicaid reimbursements are a critical source of funding to support the operation of the Indian Health system, comprised of the Indian Health Service (IHS), Tribal Health Programs, and UIOs. The federal government has a trust responsibility to provide federal health services to maintain and improve the health of AI/AN people. Due to historic underfunding of IHS, Medicaid is crucial to supporting healthcare services for AI/AN people and is critical to fulfilling the United States’ trust responsibility to maintain and improve AI/AN health.
Medicaid Coverage in AI/AN Communities
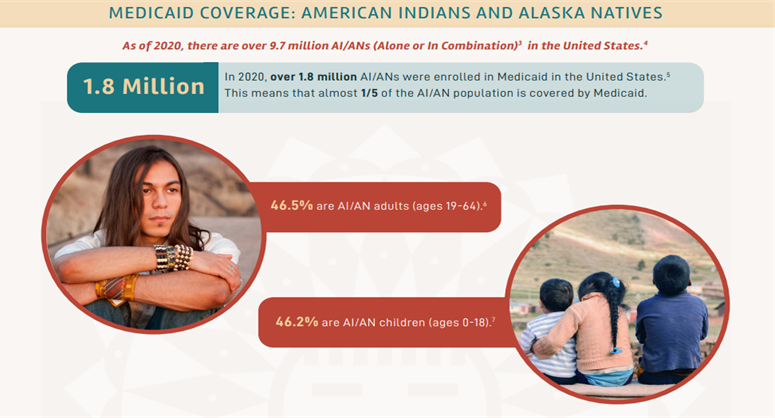
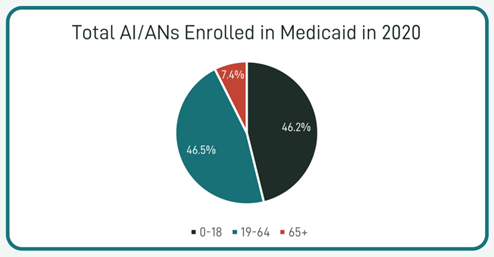
AI/AN people depend upon Medicaid to receive their healthcare coverage and services. In 2020, over 1.8 million AI/ANs were enrolled in Medicaid, meaning almost 1/5 of the AI/AN population is covered by Medicaid. Of which, 46.2% of Medicaid enrollees are AI/ANs from the ages of 0-18, and 46.5% are from the ages of 19-64.
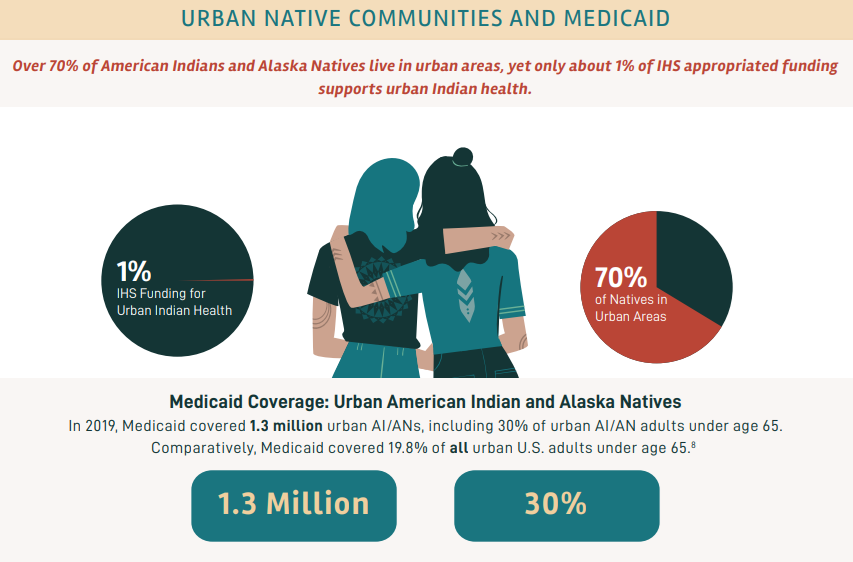
Medicaid and Urban AI/AN Communities
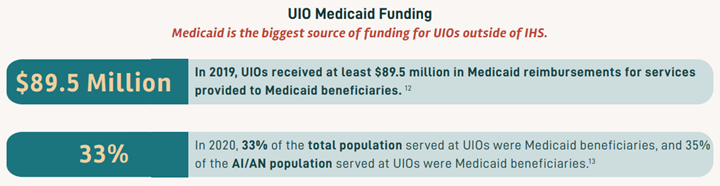
UIOs help serve the approximately 70% of AI/AN people who live in urban areas. In 2019, Medicaid covered 1.3 million urban AI/ANs, including 30% of urban AI/AN adults under the age of 65. Comparatively, Medicaid covered 19.8% of all urban U.S. adults under the age of 65.
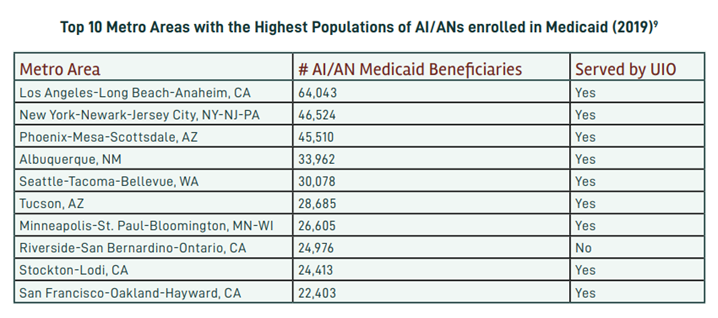
The Relocation and Termination Era and Federal Indian Boarding Schools have resulted in many AI/AN peoples living in metro areas, or cities. Below is a list of the metro areas that contain the highest population of AI/ANs who are enrolled in Medicaid. UIOs provide key services to almost all of the top metro areas where IHS-Medicaid beneficiaries live.
Medicaid: A Critical Source of Funding for Indian Health Care Providers
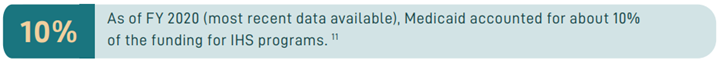
Medicaid reimbursements are a purely supplemental source of funding for IHS, as federal law prohibits appropriators from considering Medicaid revenue when determining IHS appropriations. Because the Medicaid program receives Mandatory appropriations and is not subject to the annual appropriations process, Medicaid revenue is particularly essential for Indian health providers when IHS funding is reduced or interrupted by budgetary disagreements.
Medicaid remains the largest secondary source of funding for UIO clinics. In 2020, 33% of the total population served at UIOs were Medicaid beneficiaries, and 35% of the AI/AN population served at UIOs were Medicaid beneficiaries.
Covid-19 and Medicaid Unwinding
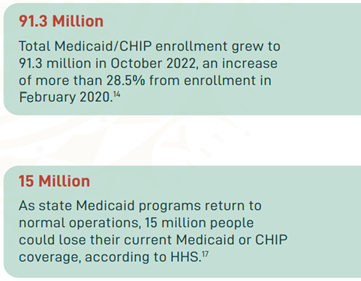 In March 2020, the Families First Coronavirus Response Act (FFCRA) Medicaid and Children’s Health Insurance Program (CHIP) “continuous coverage” requirement allowed people to retain Medicaid coverage and receive needed care during the COVID-19 Pandemic Public Health Emergency (PHE).
In March 2020, the Families First Coronavirus Response Act (FFCRA) Medicaid and Children’s Health Insurance Program (CHIP) “continuous coverage” requirement allowed people to retain Medicaid coverage and receive needed care during the COVID-19 Pandemic Public Health Emergency (PHE).
In December 2022, the Consolidated Appropriations Act, 2023 was signed into law, separating the continuous coverage provision from the COVID-19 PHE and setting an end date for the provision on March 31, 2023. This means that states may resume reviewing all Medicaid enrollees’ eligibility for coverage, a process referred to as “unwinding,” on April 1, 2023, and will begin ending coverage for those found ineligible. States must meet certain federal reporting and other requirements during the unwinding period. NCUIH recently released a Medicaid unwinding toolkit for UIOs as they prepare for changes in Medicaid coverage.

Native people may be at an increased risk of disenrollment in Medicaid and CHIP programs during the Medicaid unwinding period. In fact, Medicaid coverage losses are estimated to take twice the toll on AI/AN communities than they will take among non-Hispanic white families. It is estimated that 12% of all AI/AN children and 6% of all AI/AN adults nationwide will lose CHIP or Medicaid coverage as state Medicaid programs return to normal operations. On April 24, NCUIH and 227 other organizations sent a multi-group letter to the Department of Health and Human Services (HHS) Secretary Xavier Becerra calling on the Administration to use their full powers provided in the Consolidated Appropriations Act of 2023 to safeguard Medicaid coverage and outlines specific steps the Administration can take to avoid wrongful terminations. Inadequate health insurance coverage is a significant barrier to healthcare access, and the loss of coverage may exacerbate the significant healthcare disparities faced by AI/AN communities.