RESOURCE: COVID-19 Public Health Emergency Medicaid Unwinding Toolkit Released
The National Council of Urban Indian Health (NCUIH) recently released a Medicaid unwinding toolkit for urban Indian organizations (UIOs) as they prepare for changes in Medicaid coverage at the end of the COVID-19 pandemic Public Health Emergency (PHE). After the PHE, states will resume normal operations, which includes processing eligibility renewals and ending coverage for individuals no longer eligible for Medicaid and CHIP in a process known as “unwinding.” This document outlines the impact of Medicaid unwinding on American Indians/Alaska Natives (AI/ANs) and the steps UIOs can take to assist their patients with their coverage, such as working with their state, Tribes, federal agencies, and their community.
Background
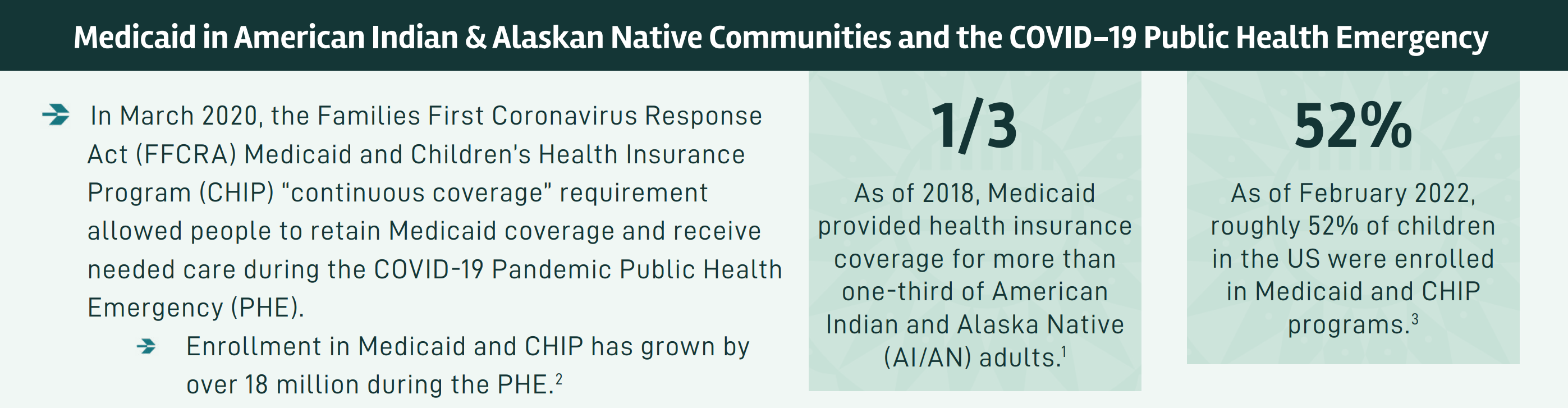
Prior to the pandemic’s PHE, Medicaid provided health insurance for more than one-third of AI/AN adults. At the beginning of the pandemic, the Families First Coronavirus Response Act (FFCRA) Medicaid and Children’s Health Insurance Program (CHIP) “continuous coverage” requirement allowed people to retain Medicaid coverage and receive needed care during the PHE.
After the PHE, states will resume normal operations, which includes processing eligibility renewals and ending coverage for individuals no longer eligible for Medicaid and CHIP in a process known as “unwinding.” According to the Department of Health and Human Services (HHS), nearly 15 million people could lose their current coverage. This will be the single largest health coverage transition event since the first open enrollment period of the Affordable Care Act (ACA). This process is expected to disproportionately impact AI/ANs, particularly those living off-reservation.
While the unwinding process will vary by state, each state will have up to 12 months to start an eligibility renewal for every individual enrolled in their entire Medicaid and CHIP population. The unwinding process will create several challenges and will result in a loss or gaps in coverage for individuals.
Impact on AI/AN Communities
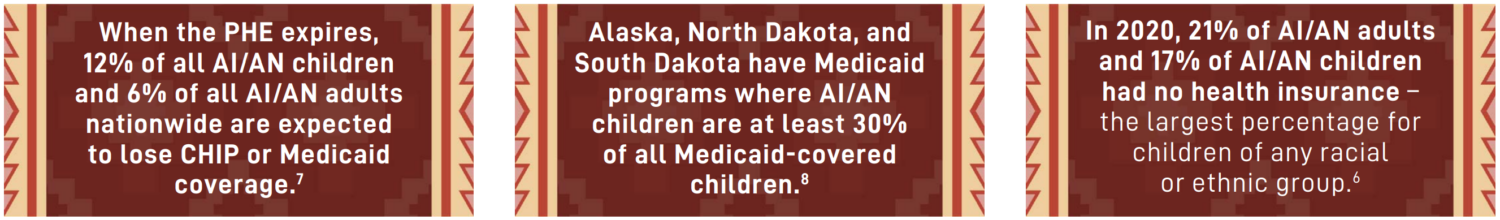
AI/ANs may be at an increased risk of disenrollment in Medicaid and CHIP programs once the PHE ends. Medicaid coverage losses are estimated to take twice the toll on AI/AN communities than they will take among non-Hispanic white families. Disenrollment of AI/ANs from Medicaid and CHIP will have significant consequences for the health and well-being of Native people – these programs are critical to fulfilling the United States’ trust responsibility to maintain and improve AI/AN health. Inadequate health insurance coverage is a significant barrier to healthcare access and often causes patients to delay or avoid medical care altogether. Alarmingly, when the PHE expires, 12% of all AI/AN children and 6% of all AI/AN adults nationwide are expected to lose CHIP or Medicaid coverage.
Medicaid-eligible AI/ANs face challenges in enrolling coverage due geographical remoteness, limited access to internet or phone service, language barriers, cultural factors, distrust of government programs, lack of knowledge of the benefits of coverage, or movement between non-reservation and reservation land.
Medicaid Unwinding and UIOs
UIOs play an important role in enrolling AI/ANs in Medicaid and CHIP as well as treating Medicaid beneficiaries, and will therefore, be critical in informing and helping eligible AI/AN maintain enrollment if eligible or explore other options. NCUIH’s resource highlights ways in which UIOs can work with states and other partners including Tribes and Tribal organizations, federal agencies like CMS and Indian Health Service (IHS), and their local communities:
Work with Your State
- Request a meeting your state regarding unwinding.
- Request that your state share renewal data via a spreadsheet or database so that you can speak with beneficiaries who utilize your services.
- Work with your state to develop targeted communication for AI/AN communities about the state’s unwinding activities.
- States can leverage Unwinding Communications Toolkit materials published by the Centers for Medicare & Medicaid Services (CMS).
- Ask your state to provide AI/AN-specific guidance on maintaining coverage through Affordable Care Act (ACA) Marketplace plans for those no longer eligible for Medicaid. AI/AN beneficiaries may have access to low-cost zero and limited cost-sharing plans on the Exchanges.
- Advocate that your state apply for Section 1902(e)(14)(a) waivers if necessary and applicable.
Work with Tribes
- Collaborate with Tribes to request a meeting with your state regarding unwinding.
- Develop partnerships with Tribes to provide necessary information to AI/AN beneficiaries.
Work with CMS, Indian Health Service (IHS), and Partner Organizations
- Request consultation and confer with CMS and IHS to discuss coverage loss concerns and oversight.
- Culturally appropriate materials are available through CMS, IHS, and the National Indian Health Board.
Work with Your Community
- Work with beneficiaries to ensure that their contact information is updated with the state Medicaid office, including addresses, emails, and phone numbers, to ensure that individuals receive information on renewals.
- Screen for potential Medicaid eligibility for all patients and refer current Medicaid recipients to your benefit specialists to update applications.
- Engage community partners, health plans, and the provider community to encourage individuals to update their contact information and to provide assistance with renewals.
- Educate patients, including utilizing outreach and educational materials in your clinic waiting rooms, patient rooms, and patient registration/in-take desks, regarding the unwinding and the risk of a loss in coverage.